Tucker Carlson discussing Ireland’s choice not to mask elementary children, Australia’s COVID martial law, school board meetings in the USA
Do Masks Work?
- First, we have to define what works means.
- If “works” is defined as “preventing infection of COVID-19“, then NO.
- Masks are a weak mitigation, but not sufficiently effective and foolproof. Under clinical conditions, the best numbers can be achieved but real world effectiveness is probably a lot lower because of mask re-use, improper mask use, substandard of counterfeit masks, and of course, the lack of N95 respirators.
- Masks didn’t do anything to stop the 1918 Spanish Flu pandemic.

Do masks make you feel safe?
- Yes. Many people believe they are protected by masks, just like kids who need a safety blanket to get to sleep.
- Feeling safe is not the same as being safe.
They are NOT effective in preventing general public from catching #Coronavirus.
-Surgeon General Jerome Adams on February 29, 2020
Folks who don’t know how to wear them properly tend to touch their faces a lot and actually can increase the spread of coronavirus.
-Surgeon General Jerome Adams on February 29, 2020 (2 days later)
During normal day-to-day activities facemasks do not provide protection from respiratory viruses, such as COVID-19 and do not need to be worn by staff.
– Public-health authorities in the United Kingdom (February 25)
There is no specific evidence to suggest that the wearing of masks by the mass population has any particular benefit.
“In fact there’s some evidence to suggest the opposite” because of the possibility of not “wearing a mask properly or fitting it properly” and of “taking it off and all the other risks that are otherwise associated with that.”
– World Health Organization (WHO) Health Emergencies Program executive director Mike Ryan (March 30, 2020)
Pandemics and Masks
- There isn’t scientific proof that masks have made any real difference in pandemic mitigation.
- Countries that never had lockdowns, never did social distancing, and never used masks did the same or better than countries that did. If these measures worked, there should have been significantly better results – there weren’t.
- Article: First randomized control trial shows face masks ‘did not reduce’ coronavirus infections with ‘statistical significance’
- In this meta-analysis, face masks were found to have no detectable effect against transmission of viral infections.
- (1 – Physical interventions to interrupt or reduce the spread of respiratory viruses. Part 1 – Face masks, eye protection and person distancing: systematic review and meta-analysis) It found: “Compared to no masks, there was Physical interventions to interrupt or reduce the spread of respiratory viruses. Part 1 – Face masks, eye protection and person distancing: systematic review and meta-analysis no reduction of influenza-like illness cases or influenza for masks in the general population, nor in healthcare workers.” source: Masks Are Neither Effective Nor Safe: A Summary Of The Science
-
This 2020 meta-analysis found that evidence from randomized controlled trials of face masks did not support a substantial effect on transmission of laboratory-confirmed influenza, either when worn by infected persons (source control) or by persons in the general community to reduce their susceptibility.(2 – Nonpharmaceutical Measures for Pandemic Influenza in Nonhealthcare Settings—Personal Protective and Environmental Measures)
-
Another recent review found that masks had no effect specifically against Covid-19, although facemask use seemed linked to, in 3 of 31 studies, “very slightly reduced” odds of developing influenza-like illness. (3 – Facemasks and similar barriers to prevent respiratory illness such as COVID-19: A rapid systematic review)
-
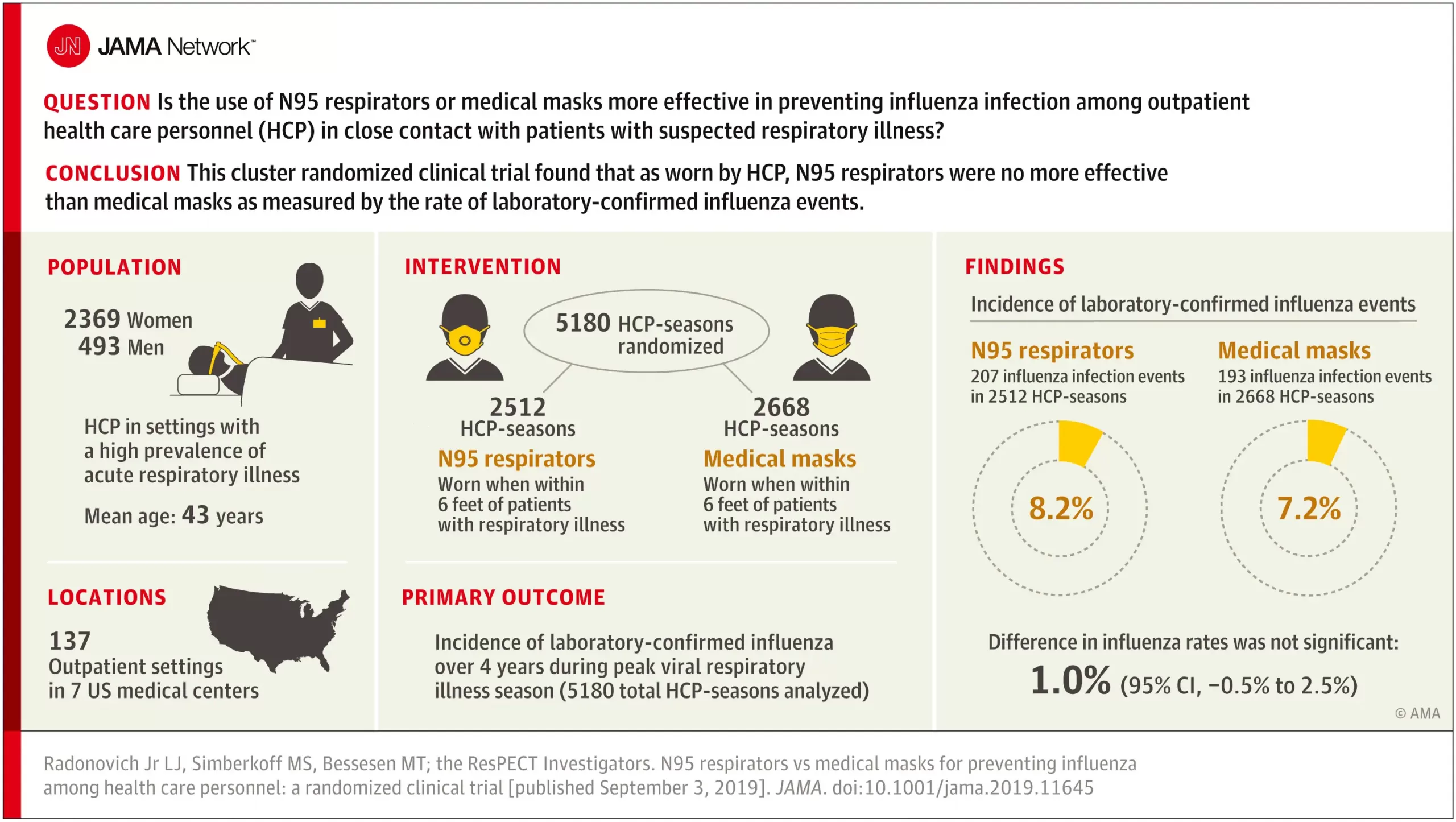
This 2019 study of 2862 participants showed that both N95 respirators and surgical masks “resulted in no significant difference in the incidence of laboratory confirmed influenza.” (4 – N95 Respirators vs Medical Masks for Preventing Influenza Among Health Care Personnel)
-
This 2016 meta-analysis found that both randomized controlled trials and observational studies of N95 respirators and surgical masks used by healthcare workers did not show benefit against transmission of acute respiratory infections. It was also found that acute respiratory infection transmission “may have occurred via contamination of provided respiratory protective equipment during storage and reuse of masks and respirators throughout the workday.” (5 – Effectiveness of N95 respirators versus surgical masks in protecting health care workers from acute respiratory infection: a systematic review and meta-analysis)
-
A 2011 meta-analysis of 17 studies regarding masks and effect on transmission of influenza found that “none of the studies established a conclusive relationship between mask/respirator use and protection against influenza infection.” (6 – The use of masks and respirators to prevent transmission of influenza: a systematic review of the scientific evidence)
-
However, authors speculated that effectiveness of masks may be linked to early, consistent and correct usage. Face mask use was likewise found to be not protective against the common cold, compared to controls without face masks among healthcare workers. (7 – Use of surgical face masks to reduce the incidence of the common cold among health care workers in Japan: a randomized controlled trial)
Masks Promote Increased Ingestion of Carbon Dioxide
- Masks also increase Carbon Dioxide consumption which is a human waste gas.
I Still Believe Masks Work – What Kind of Masks Should I Get?
- If you want better protection, get an N95 spec respirator.
- However, because of the many ways the respirator can be defeated, it should not be considered protection.
- Simply re-using, touching, or encountering contaminants will make the mask a source of contagion.
- When you encounter clouds respiratory droplets laden with SARS-CoV-2, the mask will eventually get saturated with these particles.
- The mask will turn into a sponge full of viruses and bacteria, making the mask itself a biohazard.
- This is why hospitals follow a protocol for changing them and why they change masks often. Most people won’t do this so they will not get even the marginal benefits of a hospital setting.


Airflow around masks
source: Masks Are Neither Effective Nor Safe: A Summary Of The Science
Masks have been assumed to be effective in obstructing forward travel of viral particles. Considering those positioned next to or behind a mask wearer, there have been farther transmission of virus-laden fluid particles from masked individuals than from unmasked individuals, by means of “several leakage jets, including intense backward and downwards jets that may present major hazards,” and a “potentially dangerous leakage jet of up to several meters.” (8) All masks were thought to reduce forward airflow by 90% or more over wearing no mask. However, Schlieren imaging showed that both surgical masks and cloth masks had farther brow jets (unfiltered upward airflow past eyebrows) than not wearing any mask at all, 182 mm and 203 mm respectively, vs none discernible with no mask. Backward unfiltered airflow was found to be strong with all masks compared to not masking.
For both N95 and surgical masks, it was found that expelled particles from 0.03 to 1 micron were deflected around the edges of each mask, and that there was measurable penetration of particles through the filter of each mask. (9)
Penetration through masks
A study of 44 mask brands found mean 35.6% penetration (+ 34.7%). Most medical masks had over 20% penetration, while “general masks and handkerchiefs had no protective function in terms of the aerosol filtration efficiency.” The study found that “Medical masks, general masks, and handkerchiefs were found to provide little protection against respiratory aerosols.” (10)
It may be helpful to remember that an aerosol is a colloidal suspension of liquid or solid particles in a gas. In respiration, the relevant aerosol is the suspension of bacterial or viral particles in inhaled or exhaled breath.
In another study, penetration of cloth masks by particles was almost 97% and medical masks 44%. (11)
N95 respirators
Honeywell is a manufacturer of N95 respirators. These are made with a 0.3 micron filter. (12) N95 respirators are so named, because 95% of particles having a diameter of 0.3 microns are filtered by the mask forward of the wearer, by use of an electrostatic mechanism. Coronaviruses are approximately 0.125 microns in diameter.
This meta-analysis found that N95 respirators did not provide superior protection to facemasks against viral infections or influenza-like infections. (13) This study did find superior protection by N95 respirators when they were fit-tested compared to surgical masks. (14)
This study found that 624 out of 714 people wearing N95 masks left visible gaps when putting on their own masks. (15)
Surgical masks
This study found that surgical masks offered no protection at all against influenza. (16) Another study found that surgical masks had about 85% penetration ratio of aerosolized inactivated influenza particles and about 90% of Staphylococcus aureus bacteria, although S aureus particles were about 6x the diameter of influenza particles. (17)
Use of masks in surgery were found to slightly increase incidence of infection over not masking in a study of 3,088 surgeries. (18) The surgeons’ masks were found to give no protective effect to the patients.
Other studies found no difference in wound infection rates with and without surgical masks. (19) (20)
This study found that “there is a lack of substantial evidence to support claims that facemasks protect either patient or surgeon from infectious contamination.” (21)
This study found that medical masks have a wide range of filtration efficiency, with most showing a 30% to 50% efficiency. (22)
Specifically, are surgical masks effective in stopping human transmission of coronaviruses? Both experimental and control groups, masked and unmasked respectively, were found to “not shed detectable virus in respiratory droplets or aerosols.” (23) In that study, they “did not confirm the infectivity of coronavirus” as found in exhaled breath.
A study of aerosol penetration showed that two of the five surgical masks studied had 51% to 89% penetration of polydisperse aerosols. (24)
In another study, that observed subjects while coughing, “neither surgical nor cotton masks effectively filtered SARS-CoV-2 during coughs by infected patients.” And more viral particles were found on the outside than on the inside of masks tested. (25)
Cloth masks
Cloth masks were found to have low efficiency for blocking particles of 0.3 microns and smaller. Aerosol penetration through the various cloth masks examined in this study were between 74 and 90%. Likewise, the filtration efficiency of fabric materials was 3% to 33% (26)
Healthcare workers wearing cloth masks were found to have 13 times the risk of influenza-like illness than those wearing medical masks. (27)
This 1920 analysis of cloth mask use during the 1918 pandemic examines the failure of masks to impede or stop flu transmission at that time, and concluded that the number of layers of fabric required to prevent pathogen penetration would have required a suffocating number of layers, and could not be used for that reason, as well as the problem of leakage vents around the edges of cloth masks. (28)
Masks against Covid-19
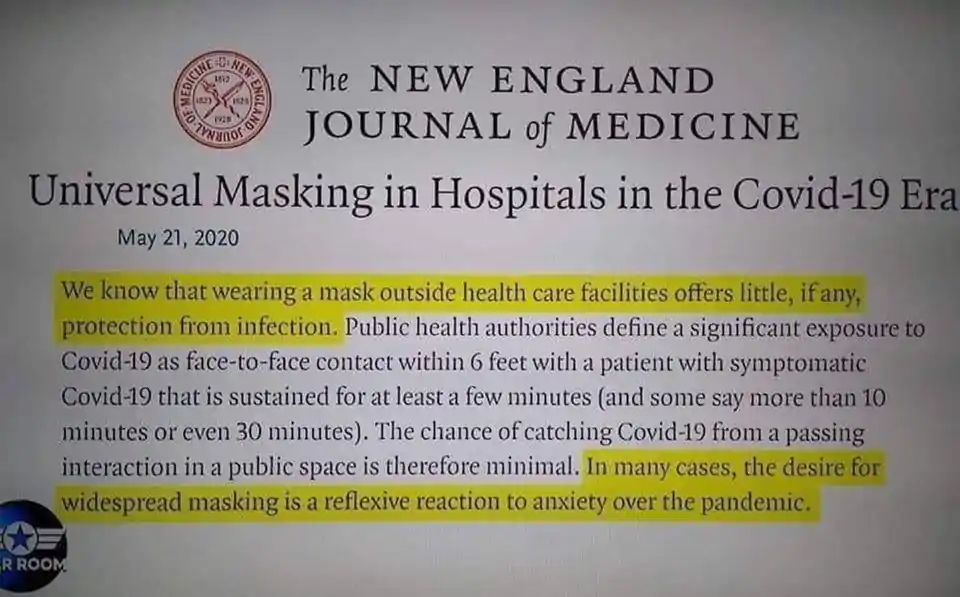
The New England Journal of Medicine editorial on the topic of mask use versus Covid-19 assesses the matter as follows:
“We know that wearing a mask outside health care facilities offers little, if any, protection from infection. Public health authorities define a significant exposure to Covid-19 as face-to-face contact within 6 feet with a patient with symptomatic Covid-19 that is sustained for at least a few minutes (and some say more than 10 minutes or even 20 minutes). The chance of catching Covid-19 from a passing interaction in a public space is therefore minimal. In many cases, the desire for widespread masking is a reflexive reaction to anxiety over the pandemic.” (29)
University of Waterloo Engineering Research
- Aerosols can infect others even more than 6 feet away (see Social Distancing).
- Previous research has found that aerosols dispersed by infected people are a source of transmission of the SARS-CoV-2 virus that causes COVID-19, even outside the two-metre social distancing zone widely recommended by public health officials.
- Common masks only filter 10% of exhaled aerosol droplets.
- N95 and KN95 (Chinese) masks filter more than 50% of exhaled aerosols.
- Modest ventilation rates were found to be as effective as the best masks.
Study: Surgical and Cloth Masks Filter Roughly 10% Efficient at Blocking Aerosols
- source: Study: Surgical and Cloth Masks Filter Roughly 10% Efficient at Blocking Aerosols
- Filter efficiency:
- Standard surgical masks – 12.4%
- Three-ply cloth masks – 9.8%
- NK95 – 46.3%
- with one-way valve: 20.3%
- loose-fitting: 3.4%
- R95 – 60.2%
- Note: N95 masks are not designed for viruses as they are too small. Filter efficiency is the result of respiratory droplets attaching to the masks, which are bigger than the virus but still too small for N95 masks to provide adequate filtration to be “protective”.
If I Want a Mask, What Should I Get?
- Do not use surgical masks – they are worse than useless.
- N95 “respirators” are the best option, although they are NOT protection.
- Although N95s are better, there are too many logistical issues such as exposure time, temporary removals, reuse, face fitment, COST, which negate their use as protection. Following a hospital protocol is extremely impractical for a weak level of mitigation and therefore no one does it. Even a single lapse in following the hospital protocol results in being exposed to a critical viral load. That makes respirators impractical as protection outside a controlled hospital environment.
- Make sure you get N95 respirators from a reputable source that meets NIOSH standards (e.g. direct from 3M or hospital supply stores).
- Watch out for fake masks.

Dr. Colin Axon
- source: Government Advisor Admits Masks Are Just “Comfort Blankets” That Do Virtually Nothing
- SAGE advisor.
- Masks have gaps in them that are up to 5000 times bigger than COVID particles.
- “Once a particle is not on a biological surface it is no longer a biomedical issue, it is simply about physics. The public has only a partial view of the story if information only comes from one type of source,” Axon continued, adding “Medics have some of the answers but not a whole view.”
- “Mask debate is about the particle journey,” Axon explained that “Masks can catch droplets and sputum from a cough but what is important is that SARS CoV-2 is predominantly distributed by tiny aerosols.”
- “A COVID viral particle is around 100 nanometres, material gaps in blue surgical masks are up to 1,000 times that size, cloth mask gaps can be 500,000 times the size,” Axon urged.
- “those aerosols escape masks and will render the mask ineffective,”
- “The public were demanding something must be done, they got masks, it is just a comfort blanket. But now it is entrenched, and we are entrenching bad behaviour.”
- “All around the world you can look at mask mandates and superimpose on infection rates, you cannot see that mask mandates made any effect whatsoever,” Axon further noted, adding that “The best thing you can say about any mask is that any positive effect they do have is too small to be measured.”
- Axon’s comments echo those of Dr. Anthony Fauci, who wrote in February 2020 that a typical store-bought face mask “is not really effective in keeping out virus, which is small enough to pass through material.”
- Fauci later reversed his position after the CDC began recommending that Americans wear face coverings. Similar recommendations were then made worldwide, with World Health Organisation officials even recommending that masks remain INDEFINTELY.
- Social media networks have long censored and deleted information pertaining to the efficacy of masks, or lack thereof, despite numerous credible studies concluding that they are largely useless at stopping the spread of COVID-19.
- Study in Denmark involving 6,000 participants found that “there was no statistically significant difference between those who wore masks and those who did not when it came to being infected by Covid-19,” the Spectator reported.
- “1.8 per cent of those wearing masks caught Covid, compared to 2.1 per cent of the control group. As a result, it seems that any effect masks have on preventing the spread of the disease in the community is small.”
Counter Argument
It’s always valuable to entertain counter arguments in case the hypothesis is wrong: https://www.kxan.com/news/coronavirus/do-face-masks-work-here-are-49-scientific-studies-that-explain-why-they-do/
Problems with Pro-Mask arguments:
- Why do un-masked countries do better or equal to masked countries in terms of cases (which are based on the discredited PCR Test) and death count?
- If masks worked, then you would see a significantly better outcomes in places that mandated masks. We didn’t see this – masks made no difference.
- “Peer reviewed” is no guarantee of scientific truth.
- Peer review simply means that a peer checked your paper for syntax and procedural correctness. This can be as superficial as checking the citation format or even just grammatical structure.
- Peer reviewed DOES NOT mean that someone reproduced the experiment and arrived at the same results, which is an absolute requirement for real science.
- That’s why scientific journals often have to retract submissions like the anti-hydroxychloroquine studies. In one case, an HCQL study was written by big-pharma lobbyists.
- The studies are sometimes nothing more than a study of other studies, looking for trends. This can be a lie based on lies.
- Anything based on “cases” is severely flawed data.
- The PCR Test, used to qualify a “case”, has been discredited by many:
- Discredited by world class lawyer Reiner Fuellmich, who prosecuted Volkswagon for their diesel emissions scam.
- The inventor of the PCR test, Kary Mullis, said that the PCR technique is not useful for diagnosing an active infection.
- The FDA recently revoked the emergency authorization of the PCR test because it is unable to diagnose the difference between Influenza and COVID-19 (SARS-CoV-2). Furthermore, how can the PCR test differentiate between SARS-CoV-2, its varients, or any other virus for that matter?
- Cases are not a scientific designation that is reproducible.
- Every country, state, county, and city counts cases differently.
- The standard for what counts is constantly changing even within the same organization.
- The CDC now wants to look for Breakthrough Cases using a PCR cycle threshold of <28 while it used to be 40. The only point in doing this is to lower the rate of positives to prove the narrative that vaccines work. If held to the same standard, the data would clearly indicate that masks don’t work.
- In many places, positive results have been found to be fraudulent for reasons other than technical error. Many places have outright falsified case results.
- There is a low standard for what is a case. You can be “believed to have COVID” to count as a case.
- Therefore, cases cannot be used to validate mask efficacy.
- The PCR Test, used to qualify a “case”, has been discredited by many:
- Studies and experiments must be properly designed.
- Many studies/experiments are controlled laboratory environments, which are not representative of real world use cases.
- Many people reuse masks indefinitely. Is this modeled in the study?
- No one replaces the mask after being exposed to a symptomatic person. Is this modeled in the study?
- Everyone uses different kinds of masks. How is this diverse product selection accounted for?
- Are atmospheric conditions modeled? Studies accomplished in southern US states naturally have lower rates of infection because people there get more sun, which produces more Vitamin D3 to strengthen their immune system.
- Are the pre-existing health of the person considered by the study?
- If you want to prove the hypothesis that “lots of people die from COVID-19”, all you have to do is find people with multiple co-morbidities (e.g. being overweight) and follow them through infection until they die.
- For example, an experiment may mist water droplets directly into a mask, but they do not measure mask leakage from every other angle. Masks are not airtight.
- The premise they prove is not the one you think.
- It’s often very limited in scope.
- e.g. the mask blocks large water droplets provided you sneeze directly into it, the mask is used only one time.
- Studies often leave out the dimension of time.
- Have mask wearing individuals been placed in an atmospherically enclosed chamber to see if they get sick from one another over a day, a week, a month?
- Study design often does not have time and place as controls. They make too many assumptions or leave out too many factors to be considered reliable. If you wanted to fraudulently prove your hypothesis in a study, just find hundreds of healthy people, put masks on them, then do a survey or test them to see if they meet the requirements for being a “case”.
- Cherry picking data is commonplace.
Employer Mask Safety Letter
Date: April, 12, 2021
To Whom It May Concern:
I am sending you this notice, related to Organization’s mask policy. My findings raise
significant concerns, both medically and legally, of the current mask policy in place. Masks are
ineffective for the purpose claimed by the mandate, potentially harmful, and only authorized for
use by an EUA.
Masks are ineffective and in many ways they harm.
It’s a myth that masks prevent viruses from spreading. The overall evidence is clear: Standard
cloth and surgical masks offer next to no protection against virus-sized particles or small aerosols.1
The size of a virus particle is much too small to be stopped by a surgical mask, cloth or bandana.
A single virion of SARS-CoV-2 is about 60-140 nanometers or 0.1 microns.2 The pore size in a
surgical mask is 200-1000x that size. Consider that the CDC website states, “surgical masks do
not catch all harmful particles in smoke.” And that the size of smoke particles in a wildfire are
~0.5 microns which is 5x the size of the SARS-CoV-2 virus! Wearing a mask to prevent catching
SARS-CoV-2, or similarly sized influenza, is like throwing sand at a chain-link fence: it doesn’t
work. There has been one large randomized controlled trial that specifically examined whether
masks protect their wearers from the coronavirus. This study found mask wearing “did not reduce,
at conventional levels of statistical significance, the incidence of Sars-Cov-2-infection.”3
Consider also, that the existence of more particles does not mean more virus. Research shows less
virus does not mean less illness. Dr. Kevin Fennelly, a pulmonologist at the National Heart, Lung
and Blood institute debunked the view that larger droplets are responsible for viral transmission.
Fennelly wrote:
“current infection control policies are based on the
premise that most respiratory infections are
transmitted by large respiratory droplets- i.e., larger
than 5 [microns] – produced by coughing and
sneezing, …Unfortunately, that premise is wrong.”4
Fennelly referenced a 1953 paper on anthrax that showed a single bacterial spore of about one
micron was significantly more lethal than larger clumps of spores.5 Exposure to one virus particle
is theoretically enough to cause infection and subsequent disease. This is not an alarming thought
– it simply means what it has always meant, that our immune system protects us continually all our
life.6
There have been hundreds of mask studies related to influenza transmission done over several
decades. It is a well-established fact that masks do not stop viruses. “Part of that evidence shows
that cloth facemasks actually increase influenza-linked illness.”7 Bacteria are 50x larger than virus
particles.8
As such, virus particles can enter through the mask pores, yet bacteria remain trapped
inside of the mask, resulting in the mask-wearer continually exposed to the bacteria.
Related to the 1918-1919 influenza pandemic, there was almost universal agreement among
experts, that deaths were virtually never caused by the influenza virus itself but resulted directly
from severe secondary pneumonia caused by well-known bacterial “pneumopathogens” that
colonized the upper respiratory tract.9 Dr. Fauci and his National Institute of Health studied
pandemics and epidemics and concluded, “the vast majority of influenza deaths resulted from
secondary bacterial pneumonia.”10
All parties mandating the use of facemasks are not only willfully ignoring established science but
are engaging in what amounts to a clinical experimental trial. This conclusion is reached by the
fact that facemask use and Covid-19 incidence are being reported in scientific opinion pieces
promoted by the CDC and others.11 The fact is after reviewing ALL of the studies worldwide,
the CDC found “no reduction in viral transmission with the use of face masks.”12
Any intervention, especially one that is prophylactic, must cause fewer harms to the recipient than
the infection. The cost-benefit of mandating an investigational face-covering with emerging safety
issues is especially difficult to justify. Anthony Fauci was very clear that asymptomatic
transmission was not a threat. He stated, “in all the history of respiratory-borne viruses of any
type, asymptomatic transmission has never been the driver of outbreaks. The driver of outbreaks
is always a symptomatic person.”13
Wearing respirators come(s) with a host of physiological and psychological burdens. These can
interfere with task performances and reduce work efficiency. These burdens can even be severe
enough to cause life-threatening conditions if not ameliorated.14 Fifteen years ago, National
Taiwan University Hospital concluded that the use of N-95 masks in healthcare workers caused
them to experience hypoxemia, a low level of oxygen in the blood, and hypercapnia, an elevation
in the blood’s carbon dioxide levels.15 Studies of simple surgical masks found significant
reductions in blood oxygen as well. In one particular study, researchers measured blood
oxygenation before and after surgeries in 53 surgeons. Researchers found the mask reduced the
blood oxygen levels significantly, and the longer the duration of wearing the mask, the greater the
drop in blood oxygen levels.16
Moreover, people with cancer will be at a further risk from hypoxia, as cancer cells grow best in a
bodily environment that is low in oxygen. Low oxygen also promotes systemic inflammation
which, in turn, promotes “the growth, invasion and spread of cancers.”17 Repeated episodes of
low oxygen, known as intermittent hypoxia, also “causes atherosclerosis” and hence increases “all
cardiovascular events” such as heart attacks, as well as adverse cerebral events like stroke.18
Informed consent is required for investigational medical therapies.
Regardless of the lack of safety and efficacy behind the decision to require employees to wear a
mask, it is illegal to mandate EUA approved investigational medical therapies without informed
consent. Mask use for viral transmission prevention is authorized for Emergency Use only.19
Emergency Use Authorization by the FDA, means “the products are investigational and
experimental” only.20 The statute granting the FDA the power to authorize a medical product of
emergency use requires that the person being administered the unapproved product be advised of
his or her right to refuse administration of the product.21 This statute further recognizes the wellsettled doctrine that medical experiments, or “clinical research,” may not be performed on human
subjects without the express, informed consent of the individual receiving treatment.22
The right to avoid the imposition of human experimentation is fundamental, rooted in the
Nuremberg Code of 1947, has been ratified by the 1964 Declaration of Helsinki, and further
codified in the United States Code of Federal Regulations. In addition to the Unites States
regarding itself as bound by these provisions, these principles were adopted by the FDA in its
regulations requiring the informed consent of human subjects for medical research.23 Add State
info here if possible. The law is very clear; It is unlawful to conduct medical research (even in the
case of emergency), unless steps taken to … secure informed consent of all participants.24
Furthermore, by requiring employees to wear a mask, you are promoting the idea that the mask can
prevent or treat a disease, which is an illegal deceptive practice. It is unlawful to advertise that a
product or service can prevent…disease unless you possess competent and reliable scientific
evidence… substantiating that the claims are true.25
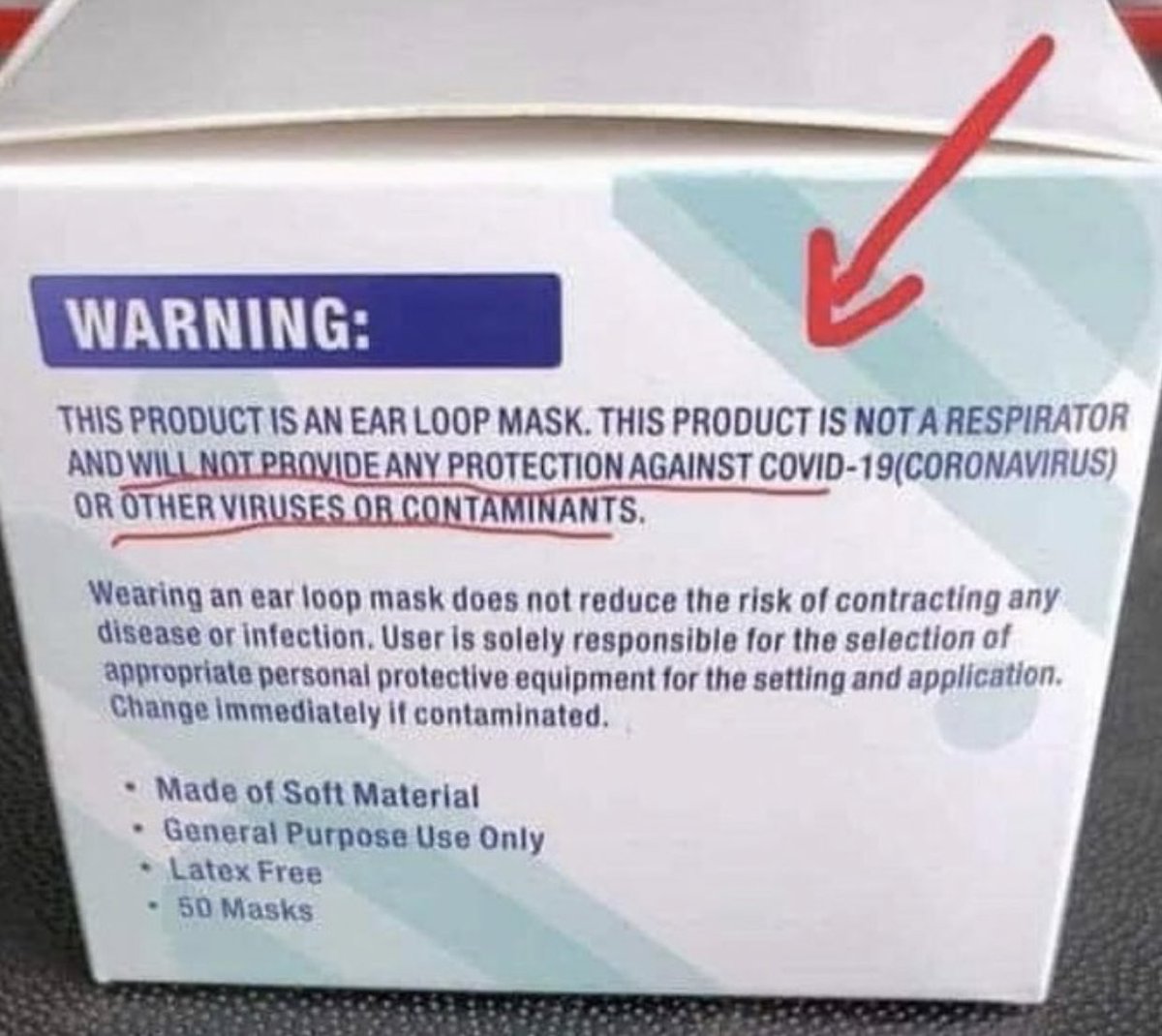
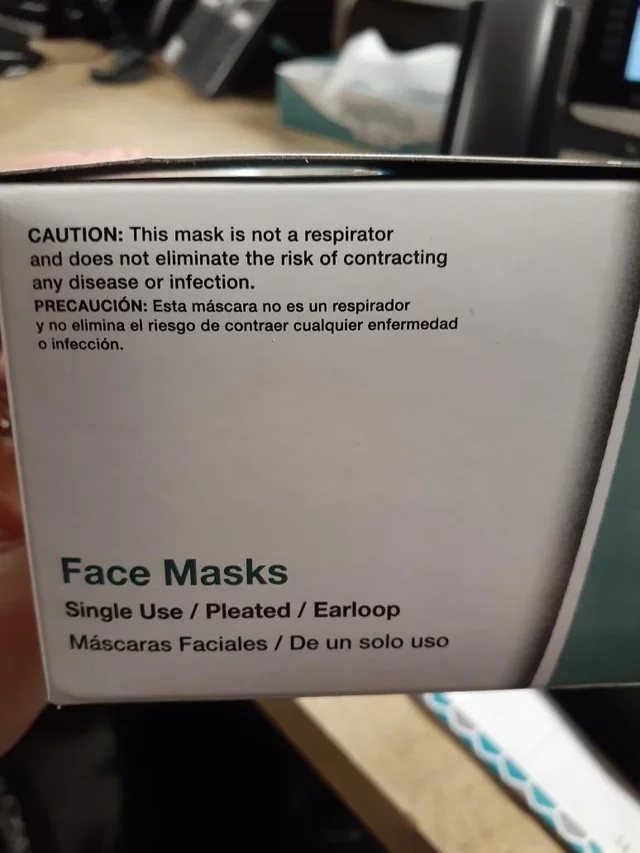
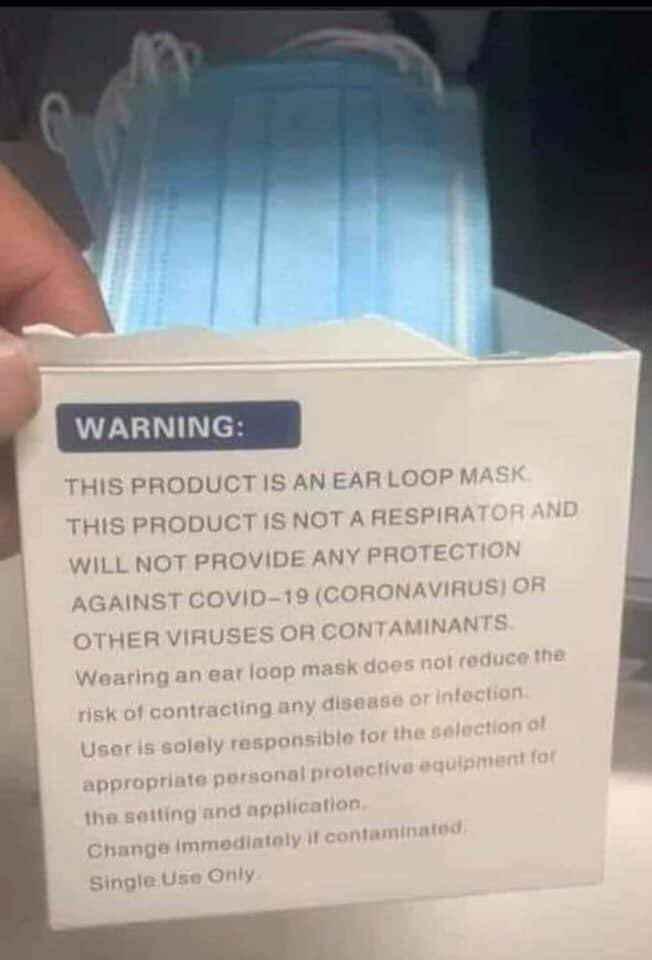
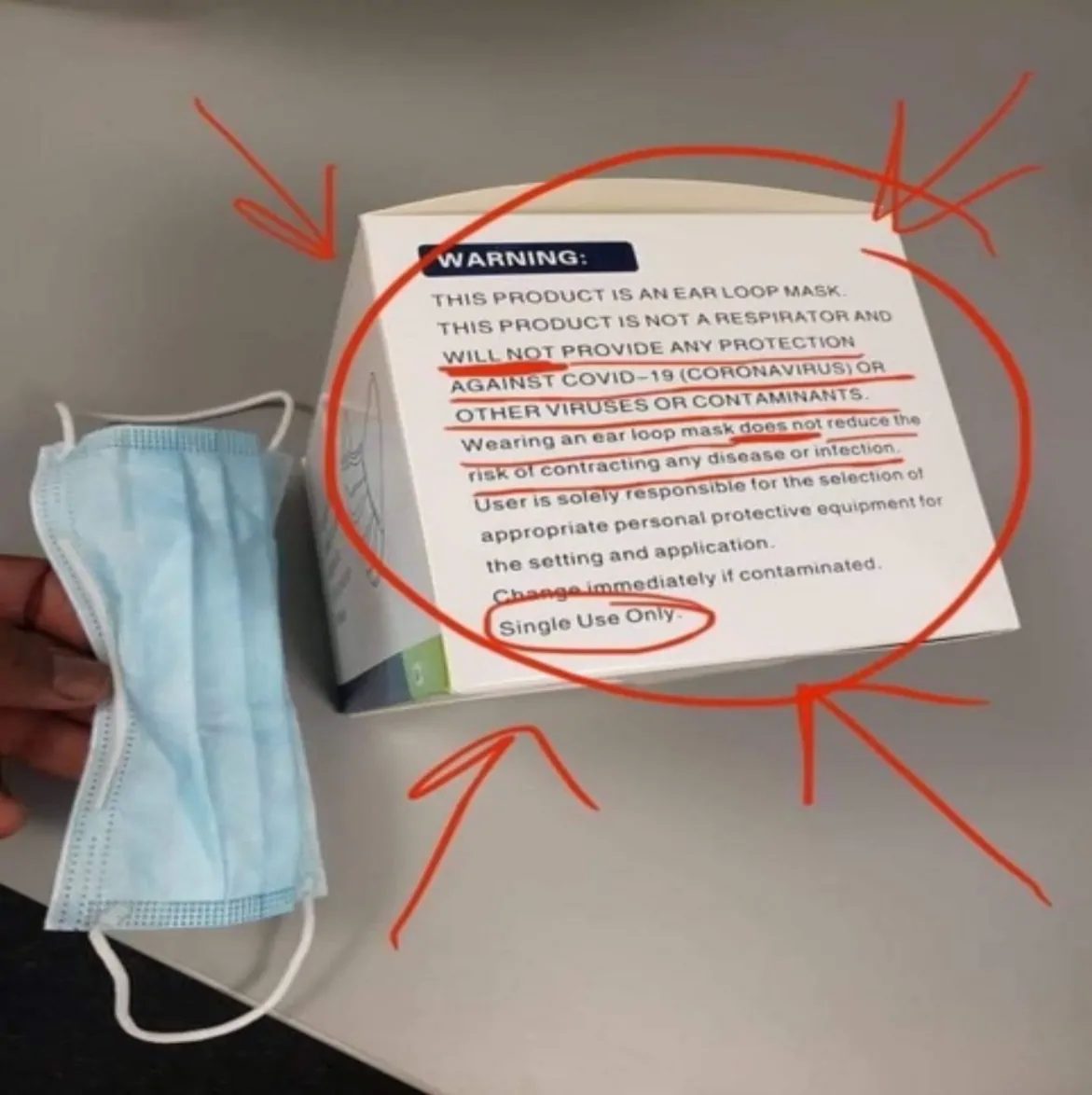
The FDA EUA for surgical and/or cloth masks explicitly states, “the labeling must not state or
imply… that the [mask] is intended for antimicrobial or antiviral protection or related, or for use
such as infection prevention or reduction.”26 As you can see from the image below, masks do not
claim to keep out viruses.
Illegally mandating an investigational medical therapy generates liability.
There are proven microbial challenges as well as breathing difficulties that are created and
exacerbated by extended mask-wearing.
Requiring employees to wear a mask sets the stage for contracting any infection, including
COVID-19, and making the consequences of that infection much graver. In essence, a mask may
very well put us at an increased risk of infection, and if so, having a far worse outcome.27
The fact that mask wearing presents a severe risk of harm to the wearer should – standing alone –
not be required for employees, particularly given that we are not ill and have done nothing wrong
that would warrant an infringement of our constitutional rights and bodily autonomy. Promoting
use of a non-FDA approved, Emergency Use Authorized mask, is unwarranted and illegal. This
mandate is in direct conflict with Section 360bbb-3€(1)(A)(ii)(I-III), which requires the wearer to
be informed of the option to refuse the wearing of such “device.” Misrepresenting the use of a
mask as being intended for antimicrobial or antiviral protection, and/or misrepresenting masks for
use as infection prevention or reduction is a deceptive practice under the FTC. It is clear, there is
no waiver of liability under deceptive practices, even under a state of emergency. As such, forcing
employees to wear masks, or similarly forcing use any other non-FDA approved medical product
without the wearer’s consent, is illegal and immoral.
This letter serves as official notice that I do not consent to being forced to wear a mask. I will not
fail to take the maximum action permissible under the law against your organization, and against
you personally. Accordingly, I urge you to comply with Federal and State law, and advise
employees they have a right to refuse or wear a mask as a measure to prevent or reduce infection
from Covid-19. Any other course of action is contrary to the law. I am willing to testify as to the
veracity of the contents in this document. Please confirm no further pressure will be exerted upon
me to follow this illegal mask mandate, and that I will not face any retaliatory disciplinary action.
Sincerely,
Name


 November 1, 2021
November 1, 2021
 October 7, 2021
October 7, 2021
 September 28, 2021
September 28, 2021
 September 25, 2021
September 25, 2021
 September 25, 2021
September 25, 2021
 September 19, 2021
September 19, 2021
 September 16, 2021
September 16, 2021