Natural immunity is the best of all forms of immunity.
– Dr. Peter McCullough
- Latest data from Israel, a country from which most CDC/FDA policies are based on has observed the following:
- Nearly 40% of new COVID patients were vaccinated.
- Under 0.0086% of new COVID patients had previous SARS-CoV-2 infection (natural immunity).
- Vaccinated people are 6.72 times more likely to get infected with SARS-CoV-2 if they were vaccinated compared to people who have natural immunity.
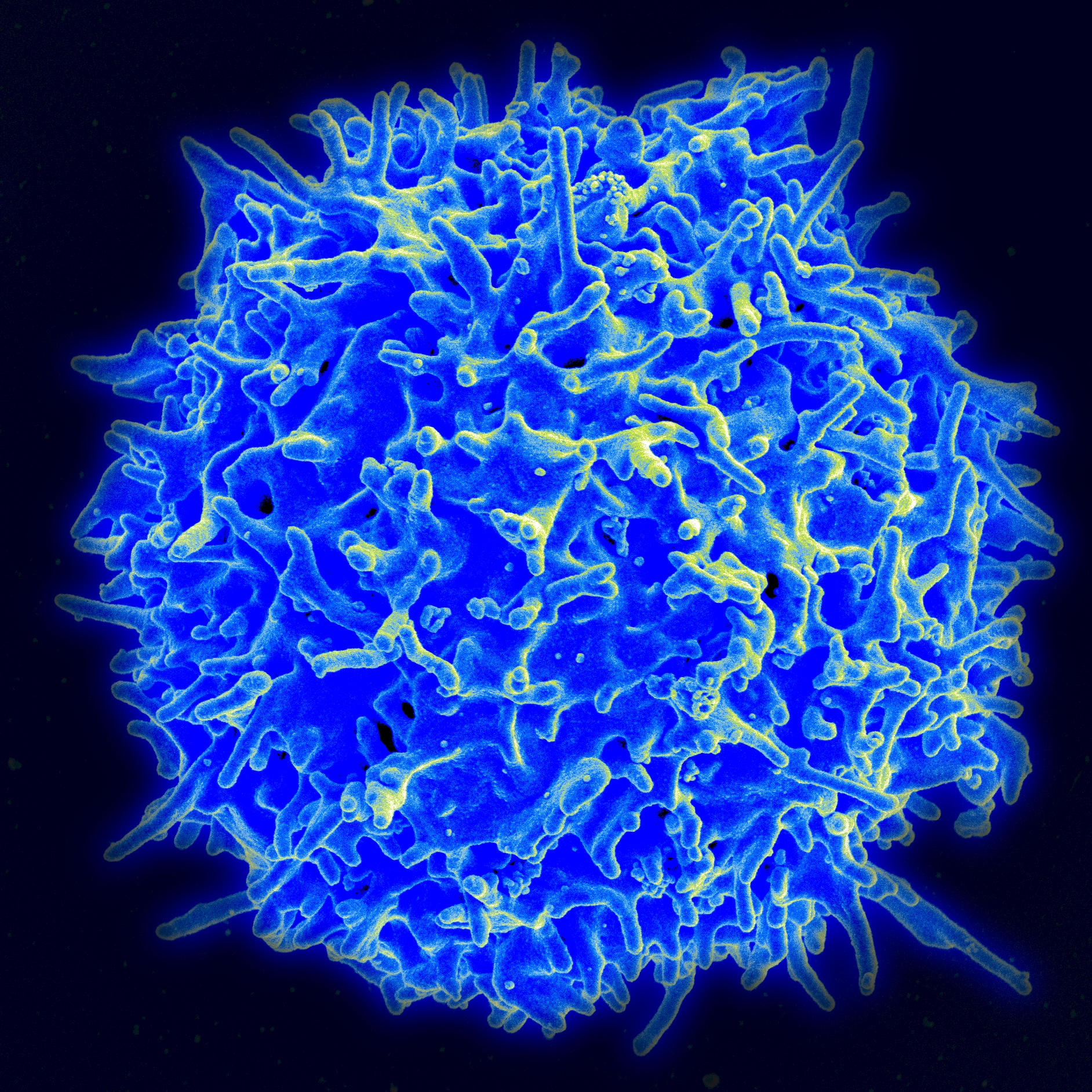
- One important component of natural immunity are T-Cells. https://askabiologist.asu.edu/t-cell
- https://www.nih.gov/news-events/nih-research-matters/antibodies-t-cells-protect-against-sars-cov-2
- They are a type of white blood cell, stronger than other defenses, that provide long term immunity beyond short lifetime antibodies.
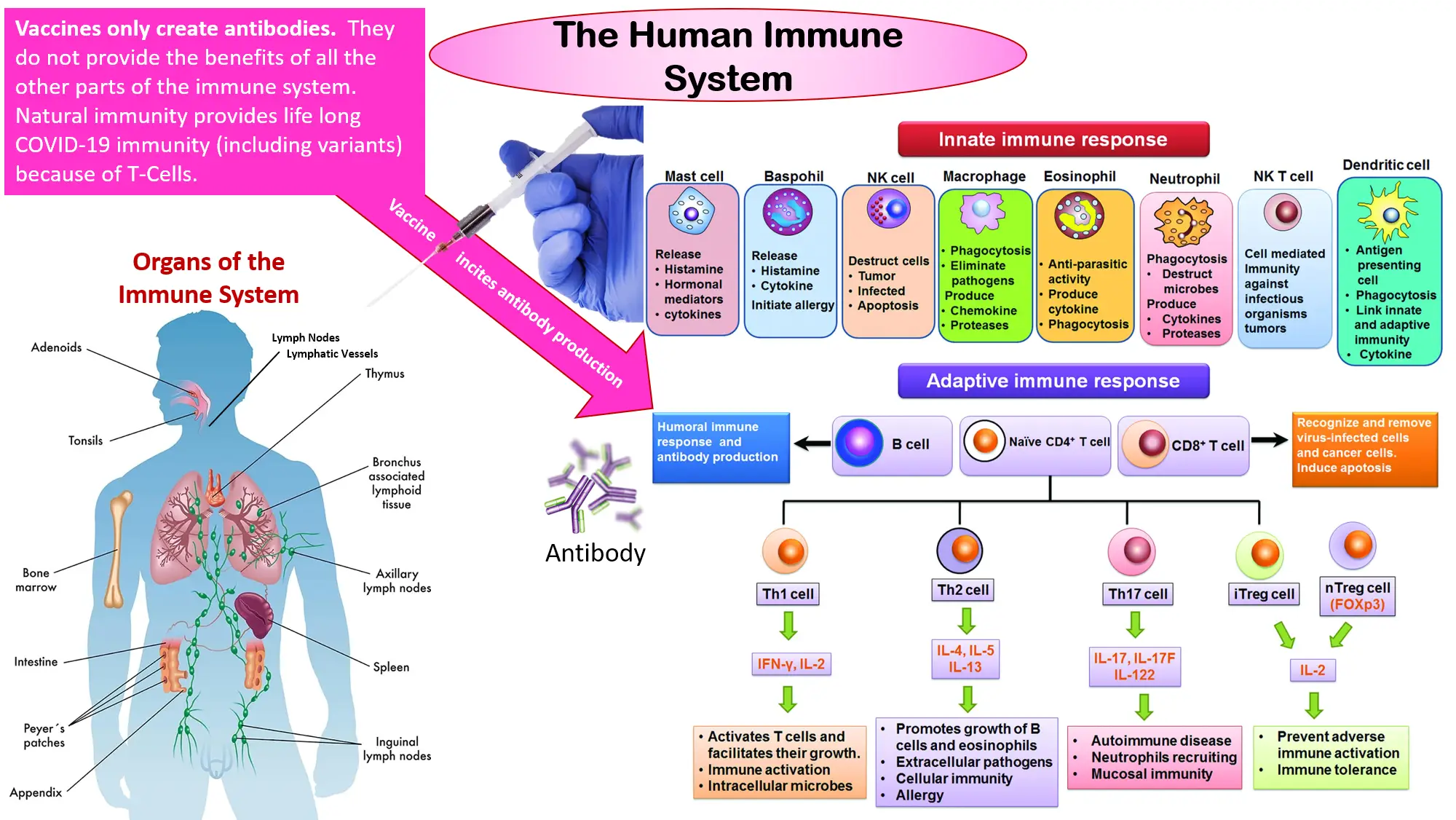
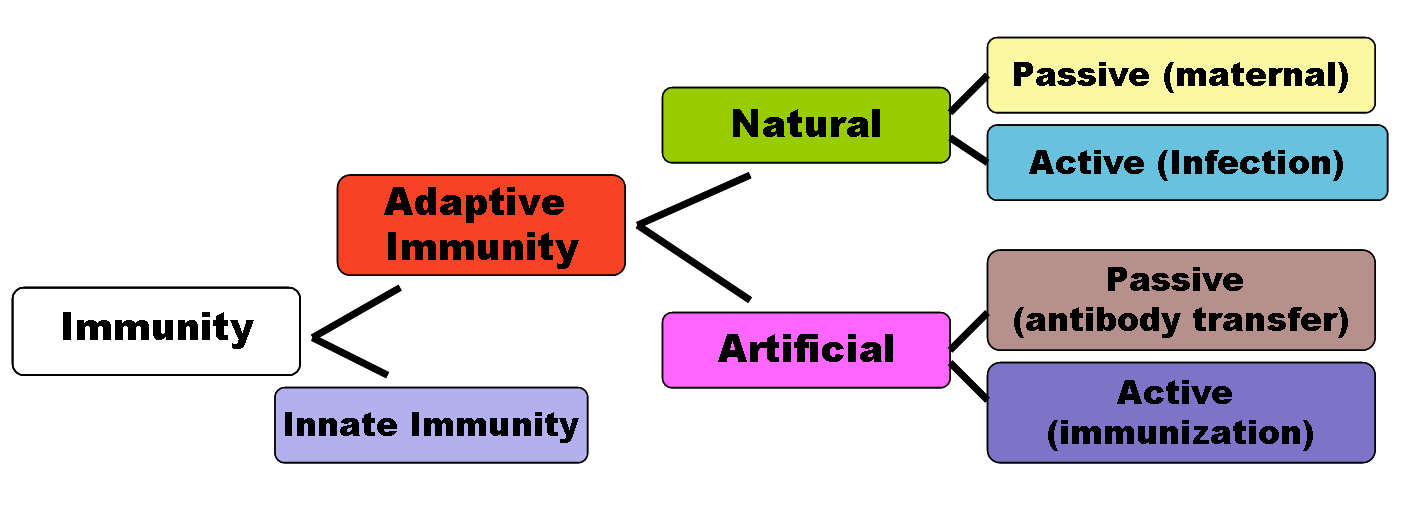
- Antibodies are produced by the human body either through infection or vaccine stimulation.
- Antibodies alone are not the entire immune system which is why vaccines are not comprehensive tools to fight infection.
- Antibodies are not produced for a long time.
- T-cells are virus specific, which makes them stronger.
- If infected with a virus, the human body fights the virus and encodes the virus into t-cells for future defense. Vaccines do not promote t-cell creation.
T-Cell
Antibodies attacking SARS-CoV-2
Studies on Effectiveness of Natural Immunity
1) New York University, May 3, 2021
The authors studied the contrast between vaccine immunity and immunity from prior infection as it relates to stimulating the innate T-cell immunity, which is more durable than adaptive immunity through antibodies alone. They concluded, “ In COVID-19 patients, immune responses were characterized by a highly augmented interferon response which was largely absent in vaccine recipients. Increased interferon signaling likely contributed to the observed dramatic upregulation of cytotoxic genes in the peripheral T cells and innate-like lymphocytes in patients but not in immunized subjects. ”
The study further notes: “Analysis of B and T cell receptor repertoires revealed that while the majority of clonal B and T cells in COVID-19 patients were effector cells, in vaccine recipients clonally expanded cells were primarily circulating memory cells.” What this means in plain English is that effector cells trigger an innate response that is quicker and more durable, whereas memory response requires an adaptive mode that is slower to respond. Natural immunity conveys much more innate immunity, while the vaccine mainly stimulates adaptive immunity.
2) Washington University, St. Louis, Missouri, May 24, 2021, published in Nature
The media scared people last year into thinking that if antibody levels wane, it means their immunity is weakening, as we are indeed seeing with the vaccines today. But as Nature wrote, “People who recover [even] from mild COVID-19 have bone-marrow cells that can churn out antibodies for decades.” Thus, aside from the robust T-cell memory that is likely lacking from most or all vaccinated individuals, prior infection creates memory B cells that “patrol the blood for reinfection, while bone marrow plasma cells (BMPCs) hide away in bones, trickling out antibodies for decades” as needed.
It’s therefore not surprising that early on in the pandemic, an in-vitro study in Singapore found the immunity against SARS-CoV-2 to last even 17 years later from SARS-1-infected patients who never even had COVID-19.
3) Cleveland Clinic, June 19, 2021
In a study of 1,359 previously infected health care workers in the Cleveland Clinic system, not a single one of them was reinfected 10 months into the pandemic, despite some of these individuals being around COVID-positive patients more than the regular population.
The study found that most recovered patients produced durable antibodies, memory B cells, and durable polyfunctional CD4 and CD8 T cells, which target multiple parts of the virus. “Taken together, these results suggest that broad and effective immunity may persist long-term in recovered COVID-19 patients ,” concluded the authors. In other words, unlike with the vaccines, no boosters are required to assist natural immunity .
5) University of California, Irvine, July 21, 2021
The authors conclude: “Natural infection induced expansion of larger CD8 T cell clones occupied distinct clusters, likely due to the recognition of a broader set of viral epitopes presented by the virus not seen in the mRNA vaccine ” (emphasis added).
6) University of California, San Francisco, May 12, 2021
Conclusion: “In infection-naïve individuals, the second dose boosted the quantity but not quality of the T cell response, while in convalescents the second dose helped neither. Spike-specific T cells from convalescent vaccinees differed strikingly from those of infection-naïve vaccinees, with phenotypic features suggesting superior long-term persistence and ability to home to the respiratory tract including the nasopharynx.”
Given that we know the virus spreads through the nasopharynx, the fact that natural infection conveys much stronger mucosal immunity makes it clear that the previously infected are much safer to be around than infection-naive people with the vaccine . The fact that this study artfully couched the choices between vaccinated naive people and vaccinated recovered rather than just plain recovered doesn’t change the fact that it’s the prior infection, not the vaccine, conveying mucosal immunity. In fact, studies now show that infected vaccinated people contain just as much viral load in their nasopharynx as those unvaccinated, a clearly unmistakable conclusion from the virus spreading wildly in many areas with nearly every adult vaccinated.
7) Israeli researchers, August 22, 2021
Aside from more robust T cell and memory B cell immunity, which is more important than antibody levels, Israeli researchers found that antibodies wane slower among those with prior infection. “In vaccinated subjects, antibody titers decreased by up to 40% each subsequent month while in convalescents they decreased by less than 5% per month.”8) Irish researchers, published in Wiley Review, May 18, 2021
Researchers conducted a review of 11 cohort studies with over 600,000 total recovered COVID patients who were followed up with over 10 months. The key finding? Unlike the vaccine, after about four to six months, they found “no study reporting an increase in the risk of reinfection over time.”
9) Cornell University, Doha, Qatar, published in the Lancet, April 27, 2021
This is one of the only studies that analyzed the population‐level risk of reinfection based on whole genome sequencing in a subset of patients with supporting evidence of reinfection. Researchers estimate the risk at 0.66 per 10,000 person-weeks. Most importantly, the study found no evidence of waning of immunity for over seven months of the follow-up period. The few reinfections that did occur “were less severe than primary infections,” and “only one reinfection was severe, two were moderate, and none were critical or fatal.” Also, unlike many vaccinated breakthrough infections in recent weeks that have been very symptomatic, “most reinfections were diagnosed incidentally through random or routine testing, or through contact tracing.”
10) Israeli researchers, April 24, 2021
Several months ago, Israeli researchers studied 6.3 million Israelis and their COVID status and were able to confirm only one death in the entire country of someone who supposedly already had the virus, and he was over 80 years old. Contrast that to the torrent of hospitalizations and deaths we are seeing in those vaccinated more than five months ago in Israel.
11) French researchers, May 11, 2021
Researchers tested blood samples from health care workers who never had the virus but got both Pfizer shots against blood samples from those health care workers who had a previous mild infection and a third group of patients who had a serious case of COVID. They found, “No neutralization escape could be feared concerning the two variants of concern [Alpha and Beta] in both populations” of those previously infected.
12) Duke-NUS Medical School, Singapore, published in Journal of Experimental Medicine
Many people are wondering: If they got only an asymptomatic infection, are they less protected against future infection than those who suffered infection with more evident symptoms? These researchers believe the opposite is true. “Asymptomatic SARS-CoV-2–infected individuals are not characterized by weak antiviral immunity; on the contrary, they mount a highly functional virus-specific cellular immune response,” wrote the authors after studying T cell responses from both symptomatic and asymptomatic convalescent patients. If anything, they found that those with asymptomatic infection only had signs of non-inflammatory cytokines, which means that the body is primed to deal with the virus without producing that dangerous inflammatory response that is killing so many hospitalized with the virus.
13) Korean researchers, published in Nature Communications on June 30, 2021
The authors found that the T cells created from convalescent patients had “stem-cell like” qualities. After studying SARS-CoV-2-specific memory T cells in recovered patients who had the virus in varying degrees of severity, the authors concluded that long-term “SARS-CoV-2-specific T cell memory is successfully maintained regardless of the severity of COVID-19 .”
14) Rockefeller University, July 29, 2021
The researchers note that far from suffering waning immunity, memory B cells in those with prior infection “express increasingly broad and potent antibodies that are resistant to mutations found in variants of concern.” They conclude that “memory antibodies selected over time by natural infection have greater potency and breadth than antibodies elicited by vaccination.” And again, this is even before getting into the innate cellular immunity which is exponentially greater in those with natural immunity.15) Researchers from Madrid and Mount Sinai, New York, March 22, 2021
Until now, we have established that natural immunity provides better adaptive B cell and innate T cell responses that last longer and work for the variants as compared to the vaccines. Moreover, those with prior infection are at greater risk for bad side effects from the vaccines, rendering the campaign to vaccinate the previously infected both unnecessary and dangerous. But the final question is: Do the vaccines possibly harm the superior T cell immunity built up from prior infection?
Immunologists from Mount Sinai in New York and Hospital La Paz in Madrid have raised serious concerns. In a shocking discovery after monitoring a group of vaccinated people both with and without prior infection, they found “in individuals with a pre-existing immunity against SARS-CoV-2, the second vaccine dose not only fail to boost humoral immunity but determines a contraction of the spike-specific T cell response.” They also note that other research has shown “the second vaccination dose appears to exert a detrimental effect in the overall magnitude of the spike-specific humoral response in COVID-19 recovered individuals.”
Natural Immunity Studies
source: 102 Research Studies Affirm Naturally Acquired Immunity to Covid-19: Documented, Linked, and Quoted
Evidence on natural immunity versus COVID-19 vaccine induced immunity as of October 15th 2021:
| Study / report title, author, and year published | Predominant finding on natural immunity |
|---|---|
| 1) Necessity of COVID-19 vaccination in previously infected individuals, Shrestha, 2021 | “Cumulative incidence of COVID-19 was examined among 52,238 employees in an American healthcare system. The cumulative incidence of SARS-CoV-2 infection remained almost zero among previously infected unvaccinated subjects, previously infected subjects who were vaccinated, and previously uninfected subjects who were vaccinated, compared with a steady increase in cumulative incidence among previously uninfected subjects who remained unvaccinated. Not one of the 1359 previously infected subjects who remained unvaccinated had a SARS-CoV-2 infection over the duration of the study. Individuals who have had SARS-CoV-2 infection are unlikely to benefit from COVID-19 vaccination…” |
| 2) SARS-CoV-2-specific T cell immunity in cases of COVID-19 and SARS, and uninfected controls, Le Bert, 2020 | “Studied T cell responses against the structural (nucleocapsid (N) protein) and non-structural (NSP7 and NSP13 of ORF1) regions of SARS-CoV-2 in individuals convalescing from coronavirus disease 2019 (COVID-19) (n = 36). In all of these individuals, we found CD4 and CD8 T cells that recognized multiple regions of the N protein…showed that patients (n = 23) who recovered from SARS possess long-lasting memory T cells that are reactive to the N protein of SARS-CoV 17 years after the outbreak of SARS in 2003; these T cells displayed robust cross-reactivity to the N protein of SARS-CoV-2.” |
| 3) Comparing SARS-CoV-2 natural immunity to vaccine-induced immunity: reinfections versus breakthrough infections,Gazit, 2021 | “A retrospective observational study comparing three groups: (1) SARS-CoV-2-naïve individuals who received a two-dose regimen of the BioNTech/Pfizer mRNA BNT162b2 vaccine, (2) previously infected individuals who have not been vaccinated, and (3) previously infected and single dose vaccinated individuals found para a 13 fold increased risk of breakthrough Delta infections in double vaccinated persons, and a 27 fold increased risk for symptomatic breakthrough infection in the double vaccinated relative to the natural immunity recovered persons…the risk of hospitalization was 8 times higher in the double vaccinated (para)…this analysis demonstrated that natural immunity affords longer lasting and stronger protection against infection, symptomatic disease and hospitalization due to the Delta variant of SARS-CoV-2, compared to the BNT162b2 two-dose vaccine-induced immunity.” |
| 4) Highly functional virus-specific cellular immune response in asymptomatic SARS-CoV-2 infection, Le Bert, 2021 | “Studied SARS-CoV-2–specific T cells in a cohort of asymptomatic (n = 85) and symptomatic (n = 75) COVID-19 patients after seroconversion…thus, asymptomatic SARS-CoV-2–infected individuals are not characterized by weak antiviral immunity; on the contrary, they mount a highly functional virus-specific cellular immune response.” |
| 5) Large-scale study of antibody titer decay following BNT162b2 mRNA vaccine or SARS-CoV-2 infection, Israel, 2021 | “A total of 2,653 individuals fully vaccinated by two doses of vaccine during the study period and 4,361 convalescent patients were included. Higher SARS-CoV-2 IgG antibody titers were observed in vaccinated individuals (median 1581 AU/mL IQR [533.8-5644.6]) after the second vaccination, than in convalescent individuals (median 355.3 AU/mL IQR [141.2-998.7]; p<0.001). In vaccinated subjects, antibody titers decreased by up to 40% each subsequent month while in convalescents they decreased by less than 5% per month…this study demonstrates individuals who received the Pfizer-BioNTech mRNA vaccine have different kinetics of antibody levels compared to patients who had been infected with the SARS-CoV-2 virus, with higher initial levels but a much faster exponential decrease in the first group”. |
| 6) SARS-CoV-2 re-infection risk in Austria, Pilz, 2021 | Researchers recorded “40 tentative re-infections in 14, 840 COVID-19 survivors of the first wave (0.27%) and 253 581 infections in 8, 885, 640 individuals of the remaining general population (2.85%) translating into an odds ratio (95% confidence interval) of 0.09 (0.07 to 0.13)…relatively low re-infection rate of SARS-CoV-2 in Austria. Protection against SARS-CoV-2 after natural infection is comparable with the highest available estimates on vaccine efficacies.” Additionally, hospitalization in only five out of 14,840 (0.03%) people and death in one out of 14,840 (0.01%) (tentative re-infection). |
| 7) mRNA vaccine-induced SARS-CoV-2-specific T cells recognize B.1.1.7 and B.1.351 variants but differ in longevity and homing properties depending on prior infection status, Neidleman, 2021 | “Spike-specific T cells from convalescent vaccinees differed strikingly from those of infection-naïve vaccinees, with phenotypic features suggesting superior long-term persistence and ability to home to the respiratory tract including the nasopharynx. These results provide reassurance that vaccine-elicited T cells respond robustly to the B.1.1.7 and B.1.351 variants, confirm that convalescents may not need a second vaccine dose.” |
| 8) Good news: Mild COVID-19 induces lasting antibody protection, Bhandari, 2021 | “Months after recovering from mild cases of COVID-19, people still have immune cells in their body pumping out antibodies against the virus that causes COVID-19, according to a study from researchers at Washington University School of Medicine in St. Louis. Such cells could persist for a lifetime, churning out antibodies all the while. The findings, published May 24 in the journal Nature, suggest that mild cases of COVID-19 leave those infected with lasting antibody protection and that repeated bouts of illness are likely to be uncommon.” |
| 9) Robust neutralizing antibodies to SARS-CoV-2 infection persist for months, Wajnberg, 2021 | “Neutralizing antibody titers against the SARS-CoV-2 spike protein persisted for at least 5 months after infection. Although continued monitoring of this cohort will be needed to confirm the longevity and potency of this response, these preliminary results suggest that the chance of reinfection may be lower than is currently feared.” |
| 10) Evolution of Antibody Immunity to SARS-CoV-2, Gaebler, 2020 | “Concurrently, neutralizing activity in plasma decreases by five-fold in pseudo-type virus assays. In contrast, the number of RBD-specific memory B cells is unchanged. Memory B cells display clonal turnover after 6.2 months, and the antibodies they express have greater somatic hypermutation, increased potency and resistance to RBD mutations, indicative of continued evolution of the humoral response…we conclude that the memory B cell response to SARS-CoV-2 evolves between 1.3 and 6.2 months after infection in a manner that is consistent with antigen persistence.” |
| 11) Persistence of neutralizing antibodies a year after SARS-CoV-2 infection in humans, Haveri, 2021 | “Assessed the persistence of serum antibodies following WT SARS-CoV-2 infection at 8 and 13 months after diagnosis in 367 individuals…found that NAb against the WT virus persisted in 89% and S-IgG in 97% of subjects for at least 13 months after infection.” |
| 12) Quantifying the risk of SARS‐CoV‐2 reinfection over time, Murchu, 2021 | “Eleven large cohort studies were identified that estimated the risk of SARS‐CoV‐2 reinfection over time, including three that enrolled healthcare workers and two that enrolled residents and staff of elderly care homes. Across studies, the total number of PCR‐positive or antibody‐positive participants at baseline was 615,777, and the maximum duration of follow‐up was more than 10 months in three studies. Reinfection was an uncommon event (absolute rate 0%–1.1%), with no study reporting an increase in the risk of reinfection over time.” |
| 13) Natural immunity to covid is powerful. Policymakers seem afraid to say so, Makary, 2021 | Makary writes “it’s okay to have an incorrect scientific hypothesis. But when new data proves it wrong, you have to adapt. Unfortunately, many elected leaders and public health officials have held on far too long to the hypothesis that natural immunity offers unreliable protection against covid-19 — a contention that is being rapidly debunked by science. More than 15 studies have demonstrated the power of immunity acquired by previously having the virus. A 700,000-person study from Israel two weeks ago found that those who had experienced prior infections were 27 times less likely to get a second symptomatic covid infection than those who were vaccinated. This affirmed a June Cleveland Clinic study of health-care workers (who are often exposed to the virus), in which none who had previously tested positive for the coronavirus got reinfected. The study authors concluded that “individuals who have had SARS-CoV-2 infection are unlikely to benefit from covid-19 vaccination.” And in May, a Washington University study found that even a mild covid infection resulted in long-lasting immunity.” |
| 14) SARS-CoV-2 elicits robust adaptive immune responses regardless of disease severity, Nielsen, 2021 | “203 recovered SARS-CoV-2 infected patients in Denmark between April 3rd and July 9th 2020, at least 14 days after COVID-19 symptom recovery… report broad serological profiles within the cohort, detecting antibody binding to other human coronaviruses… the viral surface spike protein was identified as the dominant target for both neutralizing antibodies and CD8+ T-cell responses. Overall, the majority of patients had robust adaptive immune responses, regardless of their disease severity.” |
| 15) Protection of previous SARS-CoV-2 infection is similar to that of BNT162b2 vaccine protection: A three-month nationwide experience from Israel, Goldberg, 2021 | “Analyze an updated individual-level database of the entire population of Israel to assess the protection efficacy of both prior infection and vaccination in preventing subsequent SARS-CoV-2 infection, hospitalization with COVID-19, severe disease, and death due to COVID-19… vaccination was highly effective with overall estimated efficacy for documented infection of 92·8% (CI:[92·6, 93·0]); hospitalization 94·2% (CI:[93·6, 94·7]); severe illness 94·4% (CI:[93·6, 95·0]); and death 93·7% (CI:[92·5, 94·7]). Similarly, the overall estimated level of protection from prior SARS-CoV-2 infection for documented infection is 94·8% (CI: [94·4, 95·1]); hospitalization 94·1% (CI: [91·9, 95·7]); and severe illness 96·4% (CI: [92·5, 98·3])…results question the need to vaccinate previously-infected individuals.” |
| 16) Incidence of Severe Acute Respiratory Syndrome Coronavirus-2 infection among previously infected or vaccinated employees, Kojima, 2021 | “Employees were divided into three groups: (1) SARS-CoV-2 naïve and unvaccinated, (2) previous SARS-CoV-2 infection, and (3) vaccinated. Person-days were measured from the date of the employee first test and truncated at the end of the observation period. SARS-CoV-2 infection was defined as two positive SARS-CoV-2 PCR tests in a 30-day period… 4313, 254 and 739 employee records for groups 1, 2, and 3…previous SARS-CoV-2 infection and vaccination for SARS-CoV-2 were associated with decreased risk for infection or re-infection with SARS-CoV-2 in a routinely screened workforce. The was no difference in the infection incidence between vaccinated individuals and individuals with previous infection.” |
| 17) Having SARS-CoV-2 once confers much greater immunity than a vaccine—but vaccination remains vital, Wadman, 2021 | “Israelis who had an infection were more protected against the Delta coronavirus variant than those who had an already highly effective COVID-19 vaccine…the newly released data show people who once had a SARS-CoV-2 infection were much less likely than never-infected, vaccinated people to get Delta, develop symptoms from it, or become hospitalized with serious COVID-19.” |
| 18) One-year sustained cellular and humoral immunities of COVID-19 convalescents, Zhang, 2021 | “A systematic antigen-specific immune evaluation in 101 COVID-19 convalescents; SARS-CoV-2-specific IgG antibodies, and also NAb can persist among over 95% COVID-19 convalescents from 6 months to 12 months after disease onset. At least 19/71 (26%) of COVID-19 convalescents (double positive in ELISA and MCLIA) had detectable circulating IgM antibody against SARS-CoV-2 at 12m post-disease onset. Notably, the percentages of convalescents with positive SARS-CoV-2-specific T-cell responses (at least one of the SARS-CoV-2 antigen S1, S2, M and N protein) were 71/76 (93%) and 67/73 (92%) at 6m and 12m, respectively.” |
| 19) Functional SARS-CoV-2-Specific Immune Memory Persists after Mild COVID-19, Rodda, 2021 | “Recovered individuals developed SARS-CoV-2-specific immunoglobulin (IgG) antibodies, neutralizing plasma, and memory B and memory T cells that persisted for at least 3 months. Our data further reveal that SARS-CoV-2-specific IgG memory B cells increased over time. Additionally, SARS-CoV-2-specific memory lymphocytes exhibited characteristics associated with potent antiviral function: memory T cells secreted cytokines and expanded upon antigen re-encounter, whereas memory B cells expressed receptors capable of neutralizing virus when expressed as monoclonal antibodies. Therefore, mild COVID-19 elicits memory lymphocytes that persist and display functional hallmarks of antiviral immunity.” |
| 20) Discrete Immune Response Signature to SARS-CoV-2 mRNA Vaccination Versus Infection, Ivanova, 2021 | “Performed multimodal single-cell sequencing on peripheral blood of patients with acute COVID-19 and healthy volunteers before and after receiving the SARS-CoV-2 BNT162b2 mRNA vaccine to compare the immune responses elicited by the virus and by this vaccine…both infection and vaccination induced robust innate and adaptive immune responses, our analysis revealed significant qualitative differences between the two types of immune challenges. In COVID-19 patients, immune responses were characterized by a highly augmented interferon response which was largely absent in vaccine recipients. Increased interferon signaling likely contributed to the observed dramatic upregulation of cytotoxic genes in the peripheral T cells and innate-like lymphocytes in patients but not in immunized subjects. Analysis of B and T cell receptor repertoires revealed that while the majority of clonal B and T cells in COVID-19 patients were effector cells, in vaccine recipients clonally expanded cells were primarily circulating memory cells…we observed the presence of cytotoxic CD4 T cells in COVID-19 patients that were largely absent in healthy volunteers following immunization. While hyper-activation of inflammatory responses and cytotoxic cells may contribute to immunopathology in severe illness, in mild and moderate disease, these features are indicative of protective immune responses and resolution of infection.” |
| 21) SARS-CoV-2 infection induces long-lived bone marrow plasma cells in humans, Turner, 2021 | “Bone marrow plasma cells (BMPCs) are a persistent and essential source of protective antibodies… durable serum antibody titres are maintained by long-lived plasma cells—non-replicating, antigen-specific plasma cells that are detected in the bone marrow long after the clearance of the antigen … S-binding BMPCs are quiescent, which suggests that they are part of a stable compartment. Consistently, circulating resting memory B cells directed against SARS-CoV-2 S were detected in the convalescent individuals. Overall, our results indicate that mild infection with SARS-CoV-2 induces robust antigen-specific, long-lived humoral immune memory in humans…overall, our data provide strong evidence that SARS-CoV-2 infection in humans robustly establishes the two arms of humoral immune memory: long-lived bone marrow plasma cells (BMPCs) and memory B-cells.” |
| 22) SARS-CoV-2 infection rates of antibody-positive compared with antibody-negative health-care workers in England: a large, multicentre, prospective cohort study (SIREN), Jane Hall, 2021 | “The SARS-CoV-2 Immunity and Reinfection Evaluation study… 30 625 participants were enrolled into the study… a previous history of SARS-CoV-2 infection was associated with an 84% lower risk of infection, with median protective effect observed 7 months following primary infection. This time period is the minimum probable effect because seroconversions were not included. This study shows that previous infection with SARS-CoV-2 induces effective immunity to future infections in most individuals.” |
| 23) Pandemic peak SARS-CoV-2 infection and seroconversion rates in London frontline health-care workers, Houlihan, 2020 | “Enrolled 200 patient-facing HCWs between March 26 and April 8, 2020…represents a 13% infection rate (i.e. 14 of 112 HCWs) within the 1 month of follow-up in those with no evidence of antibodies or viral shedding at enrolment. By contrast, of 33 HCWs who tested positive by serology but tested negative by RT-PCR at enrolment, 32 remained negative by RT-PCR through follow-up, and one tested positive by RT-PCR on days 8 and 13 after enrolment.” |
| 24) Antibodies to SARS-CoV-2 are associated with protection against reinfection, Lumley, 2021 | “Critical to understand whether infection with Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) protects from subsequent reinfection… 12219 HCWs participated…prior SARS-CoV-2 infection that generated antibody responses offered protection from reinfection for most people in the six months following infection.” |
| 25) Longitudinal analysis shows durable and broad immune memory after SARS-CoV-2 infection with persisting antibody responses and memory B and T cells, Cohen, 2021 | “Evaluate 254 COVID-19 patients longitudinally up to 8 months and find durable broad-based immune responses. SARS-CoV-2 spike binding and neutralizing antibodies exhibit a bi-phasic decay with an extended half-life of >200 days suggesting the generation of longer-lived plasma cells… most recovered COVID-19 patients mount broad, durable immunity after infection, spike IgG+ memory B cells increase and persist post-infection, durable polyfunctional CD4 and CD8 T cells recognize distinct viral epitope regions.” |
| 26) Single cell profiling of T and B cell repertoires following SARS-CoV-2 mRNA vaccine, Sureshchandra, 2021 | “Used single-cell RNA sequencing and functional assays to compare humoral and cellular responses to two doses of mRNA vaccine with responses observed in convalescent individuals with asymptomatic disease… natural infection induced expansion of larger CD8 T cell clones occupied distinct clusters, likely due to the recognition of a broader set of viral epitopes presented by the virus not seen in the mRNA vaccine.” |
| 27) SARS-CoV-2 antibody-positivity protects against reinfection for at least seven months with 95% efficacy, Abu-Raddad, 2021 | “SARS-CoV-2 antibody-positive persons from April 16 to December 31, 2020 with a PCR-positive swab ≥14 days after the first-positive antibody test were investigated for evidence of reinfection, 43,044 antibody-positive persons who were followed for a median of 16.3 weeks…reinfection is rare in the young and international population of Qatar. Natural infection appears to elicit strong protection against reinfection with an efficacy ~95% for at least seven months.” |
| 28) Orthogonal SARS-CoV-2 Serological Assays Enable Surveillance of Low-Prevalence Communities and Reveal Durable Humoral Immunity, Ripperger, 2020 | “Conducted a serological study to define correlates of immunity against SARS-CoV-2. Compared to those with mild coronavirus disease 2019 (COVID-19) cases, individuals with severe disease exhibited elevated virus-neutralizing titers and antibodies against the nucleocapsid (N) and the receptor binding domain (RBD) of the spike protein…neutralizing and spike-specific antibody production persists for at least 5–7 months… nucleocapsid antibodies frequently become undetectable by 5–7 months.” |
| 29) Anti-spike antibody response to natural SARS-CoV-2 infection in the general population, Wei, 2021 | “In the general population using representative data from 7,256 United Kingdom COVID-19 infection survey participants who had positive swab SARS-CoV-2 PCR tests from 26-April-2020 to 14-June-2021…we estimated antibody levels associated with protection against reinfection likely last 1.5-2 years on average, with levels associated with protection from severe infection present for several years. These estimates could inform planning for vaccination booster strategies.” |
| 30) Antibody Status and Incidence of SARS-CoV-2 Infection in Health Care Workers, Lumley, 2021 | “12,541 health care workers participated and had anti-spike IgG measured; 11,364 were followed up after negative antibody results and 1265 after positive results, including 88 in whom seroconversion occurred during follow-up…a total of 223 anti-spike–seronegative health care workers had a positive PCR test (1.09 per 10,000 days at risk), 100 during screening while they were asymptomatic and 123 while symptomatic, whereas 2 anti-spike–seropositive health care workers had a positive PCR test… the presence of anti-spike or anti-nucleocapsid IgG antibodies was associated with a substantially reduced risk of SARS-CoV-2 reinfection in the ensuing 6 months.” |
| 31) Researchers find long-lived immunity to 1918 pandemic virus, CIDRAP, 2008 and the actual 2008 NATURE journal publication by Yu |
“A study of the blood of older people who survived the 1918 influenza pandemic reveals that antibodies to the strain have lasted a lifetime and can perhaps be engineered to protect future generations against similar strains…the group collected blood samples from 32 pandemic survivors aged 91 to 101..the people recruited for the study were 2 to 12 years old in 1918 and many recalled sick family members in their households, which suggests they were directly exposed to the virus, the authors report. The group found that 100% of the subjects had serum-neutralizing activity against the 1918 virus and 94% showed serologic reactivity to the 1918 hemagglutinin. The investigators generated B lymphoblastic cell lines from the peripheral blood mononuclear cells of eight subjects. Transformed cells from the blood of 7 of the 8 donors yielded secreting antibodies that bound the 1918 hemagglutinin.” Yu: “here we show that of the 32 individuals tested that were born in or before 1915, each showed sero-reactivity with the 1918 virus, nearly 90 years after the pandemic. Seven of the eight donor samples tested had circulating B cells that secreted antibodies that bound the 1918 HA. We isolated B cells from subjects and generated five monoclonal antibodies that showed potent neutralizing activity against 1918 virus from three separate donors. These antibodies also cross-reacted with the genetically similar HA of a 1930 swine H1N1 influenza strain.” |
| 32) Live virus neutralisation testing in convalescent patients and subjects vaccinated against 19A, 20B, 20I/501Y.V1 and 20H/501Y.V2 isolates of SARS-CoV-2, Gonzalez, 2021 | “No significant difference was observed between the 20B and 19A isolates for HCWs with mild COVID-19 and critical patients. However, a significant decrease in neutralisation ability was found for 20I/501Y.V1 in comparison with 19A isolate for critical patients and HCWs 6-months post infection. Concerning 20H/501Y.V2, all populations had a significant reduction in neutralising antibody titres in comparison with the 19A isolate. Interestingly, a significant difference in neutralisation capacity was observed for vaccinated HCWs between the two variants whereas it was not significant for the convalescent groups…the reduced neutralising response observed towards the 20H/501Y.V2 in comparison with the 19A and 20I/501Y.V1 isolates in fully immunized subjects with the BNT162b2 vaccine is a striking finding of the study.” |
| 33) Differential effects of the second SARS-CoV-2 mRNA vaccine dose on T cell immunity in naïve and COVID-19 recovered individuals, Camara, 2021 | “Characterized SARS-CoV-2 spike-specific humoral and cellular immunity in naïve and previously infected individuals during full BNT162b2 vaccination…results demonstrate that the second dose increases both the humoral and cellular immunity in naïve individuals. On the contrary, the second BNT162b2 vaccine dose results in a reduction of cellular immunity in COVID-19 recovered individuals.” |
| 34) Op-Ed: Quit Ignoring Natural COVID Immunity, Klausner, 2021 | “Epidemiologists estimate over 160 million people worldwide have recovered from COVID-19. Those who have recovered have an astonishingly low frequency of repeat infection, disease, or death.” |
| 35) Association of SARS-CoV-2 Seropositive Antibody Test With Risk of Future Infection, Harvey, 2021 | “To evaluate evidence of SARS-CoV-2 infection based on diagnostic nucleic acid amplification test (NAAT) among patients with positive vs negative test results for antibodies in an observational descriptive cohort study of clinical laboratory and linked claims data…the cohort included 3 257 478 unique patients with an index antibody test…patients with positive antibody test results were initially more likely to have positive NAAT results, consistent with prolonged RNA shedding, but became markedly less likely to have positive NAAT results over time, suggesting that seropositivity is associated with protection from infection.” |
| 36) SARS-CoV-2 seropositivity and subsequent infection risk in healthy young adults: a prospective cohort study, Letizia, 2021 | “Investigated the risk of subsequent SARS-CoV-2 infection among young adults (CHARM marine study) seropositive for a previous infection…enrolled 3249 participants, of whom 3168 (98%) continued into the 2-week quarantine period. 3076 (95%) participants…Among 189 seropositive participants, 19 (10%) had at least one positive PCR test for SARS-CoV-2 during the 6-week follow-up (1·1 cases per person-year). In contrast, 1079 (48%) of 2247 seronegative participants tested positive (6·2 cases per person-year). The incidence rate ratio was 0·18 (95% CI 0·11–0·28; p<0·001)…infected seropositive participants had viral loads that were about 10-times lower than those of infected seronegative participants (ORF1ab gene cycle threshold difference 3·95 [95% CI 1·23–6·67]; p=0·004).” |
| 37) Associations of Vaccination and of Prior Infection With Positive PCR Test Results for SARS-CoV-2 in Airline Passengers Arriving in Qatar, Bertollini, 2021 | “Of 9,180 individuals with no record of vaccination but with a record of prior infection at least 90 days before the PCR test (group 3), 7694 could be matched to individuals with no record of vaccination or prior infection (group 2), among whom PCR positivity was 1.01% (95% CI, 0.80%-1.26%) and 3.81% (95% CI, 3.39%-4.26%), respectively. The relative risk for PCR positivity was 0.22 (95% CI, 0.17-0.28) for vaccinated individuals and 0.26 (95% CI, 0.21-0.34) for individuals with prior infection compared with no record of vaccination or prior infection.” |
| 38) Natural immunity against COVID-19 significantly reduces the risk of reinfection: findings from a cohort of sero-survey participants, Mishra, 2021 | “Followed up with a subsample of our previous sero-survey participants to assess whether natural immunity against SARS-CoV-2 was associated with a reduced risk of re-infection (India)… out of the 2238 participants, 1170 were sero-positive and 1068 were sero-negative for antibody against COVID-19. Our survey found that only 3 individuals in the sero-positive group got infected with COVID-19 whereas 127 individuals reported contracting the infection the sero-negative group…from the 3 sero-positives re-infected with COVID-19, one had hospitalization, but did not require oxygen support or critical care…development of antibody following natural infection not only protects against re-infection by the virus to a great extent, but also safeguards against progression to severe COVID-19 disease.” |
| 39) Lasting immunity found after recovery from COVID-19, NIH, 2021 | “The researchers found durable immune responses in the majority of people studied. Antibodies against the spike protein of SARS-CoV-2, which the virus uses to get inside cells, were found in 98% of participants one month after symptom onset. As seen in previous studies, the number of antibodies ranged widely between individuals. But, promisingly, their levels remained fairly stable over time, declining only modestly at 6 to 8 months after infection… virus-specific B cells increased over time. People had more memory B cells six months after symptom onset than at one month afterwards… levels of T cells for the virus also remained high after infection. Six months after symptom onset, 92% of participants had CD4+ T cells that recognized the virus… 95% of the people had at least 3 out of 5 immune-system components that could recognize SARS-CoV-2 up to 8 months after infection.” |
| 40) SARS-CoV-2 Natural Antibody Response Persists for at Least 12 Months in a Nationwide Study From the Faroe Islands, Petersen, 2021 | “The seropositive rate in the convalescent individuals was above 95% at all sampling time points for both assays and remained stable over time; that is, almost all convalescent individuals developed antibodies… results show that SARS-CoV-2 antibodies persisted at least 12 months after symptom onset and maybe even longer, indicating that COVID-19-convalescent individuals may be protected from reinfection.” |
| 41) SARS-CoV-2-specific T cell memory is sustained in COVID-19 convalescent patients for 10 months with successful development of stem cell-like memory T cells, Jung, 2021 | “ex vivo assays to evaluate SARS-CoV-2-specific CD4+ and CD8+ T cell responses in COVID-19 convalescent patients up to 317 days post-symptom onset (DPSO), and find that memory T cell responses are maintained during the study period regardless of the severity of COVID-19. In particular, we observe sustained polyfunctionality and proliferation capacity of SARS-CoV-2-specific T cells. Among SARS-CoV-2-specific CD4+ and CD8+ T cells detected by activation-induced markers, the proportion of stem cell-like memory T (TSCM) cells is increased, peaking at approximately 120 DPSO.” |
| 42) Immune Memory in Mild COVID-19 Patients and Unexposed Donors Reveals Persistent T Cell Responses After SARS-CoV-2 Infection, Ansari, 2021 | “Analyzed 42 unexposed healthy donors and 28 mild COVID-19 subjects up to 5 months from the recovery for SARS-CoV-2 specific immunological memory. Using HLA class II predicted peptide megapools, we identified SARS-CoV-2 cross-reactive CD4+ T cells in around 66% of the unexposed individuals. Moreover, we found detectable immune memory in mild COVID-19 patients several months after recovery in the crucial arms of protective adaptive immunity; CD4+ T cells and B cells, with a minimal contribution from CD8+ T cells. Interestingly, the persistent immune memory in COVID-19 patients is predominantly targeted towards the Spike glycoprotein of the SARS-CoV-2. This study provides the evidence of both high magnitude pre-existing and persistent immune memory in Indian population.” |
| 43) COVID-19 natural immunity, WHO, 2021 | “Current evidence points to most individuals developing strong protective immune responses following natural infection with SARSCoV-2. Within 4 weeks following infection, 90-99% of individuals infected with the SARS-CoV-2 virus develop detectable neutralizing antibodies. The strength and duration of the immune responses to SARS-CoV-2 are not completely understood and currently available data suggests that it varies by age and the severity of symptoms. Available scientific data suggests that in most people immune responses remain robust and protective against reinfection for at least 6-8 months after infection (the longest follow up with strong scientific evidence is currently approximately 8 months).” |
| 44) Antibody Evolution after SARS-CoV-2 mRNA Vaccination, Cho, 2021 | “We conclude that memory antibodies selected over time by natural infection have greater potency and breadth than antibodies elicited by vaccination…boosting vaccinated individuals with currently available mRNA vaccines would produce a quantitative increase in plasma neutralizing activity but not the qualitative advantage against variants obtained by vaccinating convalescent individuals.” |
| 45) Humoral Immune Response to SARS-CoV-2 in Iceland, Gudbjartsson, 2020 | “Measured antibodies in serum samples from 30,576 persons in Iceland…of the 1797 persons who had recovered from SARS-CoV-2 infection, 1107 of the 1215 who were tested (91.1%) were seropositive…results indicate risk of death from infection was 0.3% and that antiviral antibodies against SARS-CoV-2 did not decline within 4 months after diagnosis (para).” |
| 46) Immunological memory to SARS-CoV-2 assessed for up to 8 months after infection, Dan, 2021 | “Analyzed multiple compartments of circulating immune memory to SARS-CoV-2 in 254 samples from 188 COVID-19 cases, including 43 samples at ≥ 6 months post-infection…IgG to the Spike protein was relatively stable over 6+ months. Spike-specific memory B cells were more abundant at 6 months than at 1 month post symptom onset.” |
| 47) The prevalence of adaptive immunity to COVID-19 and reinfection after recovery – a comprehensive systematic review and meta-analysis of 12 011 447 individuals, Chivese, 2021 | “Fifty-four studies, from 18 countries, with a total of 12 011 447 individuals, followed up to 8 months after recovery, were included. At 6-8 months after recovery, the prevalence of detectable SARS-CoV-2 specific immunological memory remained high; IgG – 90.4%… pooled prevalence of reinfection was 0.2% (95%CI 0.0 – 0.7, I2 = 98.8, 9 studies). Individuals who recovered from COVID-19 had an 81% reduction in odds of a reinfection (OR 0.19, 95% CI 0.1 – 0.3, I2 = 90.5%, 5 studies).” |
| 48) Reinfection Rates among Patients who Previously Tested Positive for COVID-19: a Retrospective Cohort Study, Sheehan, 2021 | “Retrospective cohort study of one multi-hospital health system included 150,325 patients tested for COVID-19 infection…prior infection in patients with COVID-19 was highly protective against reinfection and symptomatic disease. This protection increased over time, suggesting that viral shedding or ongoing immune response may persist beyond 90 days and may not represent true reinfection.” |
| 49) Assessment of SARS-CoV-2 Reinfection 1 Year After Primary Infection in a Population in Lombardy, Italy, Vitale, 2020 | “The study results suggest that reinfections are rare events and patients who have recovered from COVID-19 have a lower risk of reinfection. Natural immunity to SARS-CoV-2 appears to confer a protective effect for at least a year, which is similar to the protection reported in recent vaccine studies.” |
| 50) Prior SARS-CoV-2 infection is associated with protection against symptomatic reinfection, Hanrath, 2021 | “We observed no symptomatic reinfections in a cohort of healthcare workers…this apparent immunity to re-infection was maintained for at least 6 months…test positivity rates were 0% (0/128 [95% CI: 0–2.9]) in those with previous infection compared to 13.7% (290/2115 [95% CI: 12.3–15.2]) in those without (P<0.0001 χ2 test).” |
| 51) mRNA vaccine-induced T cells respond identically to SARS-CoV-2 variants of concern but differ in longevity and homing properties depending on prior infection status, Neidleman, 2021 | “In infection-naïve individuals, the second dose boosted the quantity and altered the phenotypic properties of SARS-CoV-2-specific T cells, while in convalescents the second dose changed neither. Spike-specific T cells from convalescent vaccinees differed strikingly from those of infection-naïve vaccinees, with phenotypic features suggesting superior long-term persistence and ability to home to the respiratory tract including the nasopharynx.” |
| 52) Targets of T Cell Responses to SARS-CoV-2 Coronavirus in Humans with COVID-19 Disease and Unexposed Individuals, Grifoni, 2020 | “Using HLA class I and II predicted peptide “megapools,” circulating SARS-CoV-2-specific CD8+ and CD4+ T cells were identified in ∼70% and 100% of COVID-19 convalescent patients, respectively. CD4+ T cell responses to spike, the main target of most vaccine efforts, were robust and correlated with the magnitude of the anti-SARS-CoV-2 IgG and IgA titers. The M, spike, and N proteins each accounted for 11%–27% of the total CD4+ response, with additional responses commonly targeting nsp3, nsp4, ORF3a, and ORF8, among others. For CD8+ T cells, spike and M were recognized, with at least eight SARS-CoV-2 ORFs targeted.” |
| 53) NIH Director’s Blog: Immune T Cells May Offer Lasting Protection Against COVID-19, Collins, 2021 | “Much of the study on the immune response to SARS-CoV-2, the novel coronavirus that causes COVID-19, has focused on the production of antibodies. But, in fact, immune cells known as memory T cells also play an important role in the ability of our immune systems to protect us against many viral infections, including—it now appears—COVID-19.An intriguing new study of these memory T cells suggests they might protect some people newly infected with SARS-CoV-2 by remembering past encounters with other human coronaviruses. This might potentially explain why some people seem to fend off the virus and may be less susceptible to becoming severely ill with COVID-19.” |
| 54) Ultrapotent antibodies against diverse and highly transmissible SARS-CoV-2 variants, Wang, 2021 | “Our study demonstrates that convalescent subjects previously infected with ancestral variant SARS-CoV-2 produce antibodies that cross-neutralize emerging VOCs with high potency…potent against 23 variants, including variants of concern.” |
| 55) Why COVID-19 Vaccines Should Not Be Required for All Americans, Makary, 2021 | “Requiring the vaccine in people who are already immune with natural immunity has no scientific support. While vaccinating those people may be beneficial – and it’s a reasonable hypothesis that vaccination may bolster the longevity of their immunity – to argue dogmatically that they must get vaccinated has zero clinical outcome data to back it. As a matter of fact, we have data to the contrary: A Cleveland Clinic study found that vaccinating people with natural immunity did not add to their level of protection.” |
| 56) Protracted yet coordinated differentiation of long-lived SARS-CoV-2-specific CD8+ T cells during COVID-19 convalescence, Ma, 2021 | “Screened 21 well-characterized, longitudinally-sampled convalescent donors that recovered from mild COVID-19…following a typical case of mild COVID-19, SARS-CoV-2-specific CD8+ T cells not only persist but continuously differentiate in a coordinated fashion well into convalescence, into a state characteristic of long-lived, self-renewing memory.” |
| 57) Decrease in Measles Virus-Specific CD4 T Cell Memory in Vaccinated Subjects, Naniche, 2004 | “Characterized the profiles of measles vaccine (MV) vaccine-induced antigen-specific T cells over time since vaccination. In a cross-sectional study of healthy subjects with a history of MV vaccination, we found that MV-specific CD4 and CD8 T cells could be detected up to 34 years after vaccination. The levels of MV-specific CD8 T cells and MV-specific IgG remained stable, whereas the level of MV-specific CD4 T cells decreased significantly in subjects who had been vaccinated >21 years earlier.” |
| 58) Remembrance of Things Past: Long-Term B Cell Memory After Infection and Vaccination, Palm, 2019 | “The success of vaccines is dependent on the generation and maintenance of immunological memory. The immune system can remember previously encountered pathogens, and memory B and T cells are critical in secondary responses to infection. Studies in mice have helped to understand how different memory B cell populations are generated following antigen exposure and how affinity for the antigen is determinant to B cell fate… upon re-exposure to an antigen the memory recall response will be faster, stronger, and more specific than a naïve response. Protective memory depends first on circulating antibodies secreted by LLPCs. When these are not sufficient for immediate pathogen neutralization and elimination, memory B cells are recalled.” |
| 59) SARS-CoV-2 specific memory B-cells from individuals with diverse disease severities recognize SARS-CoV-2 variants of concern, Lyski, 2021 | “Examined the magnitude, breadth, and durability of SARS-CoV-2 specific antibodies in two distinct B-cell compartments: long-lived plasma cell-derived antibodies in the plasma, and peripheral memory B-cells along with their associated antibody profiles elicited after in vitro stimulation. We found that magnitude varied amongst individuals, but was the highest in hospitalized subjects. Variants of concern (VoC) -RBD-reactive antibodies were found in the plasma of 72% of samples in this investigation, and VoC-RBD-reactive memory B-cells were found in all but 1 subject at a single time-point. This finding, that VoC-RBD-reactive MBCs are present in the peripheral blood of all subjects including those that experienced asymptomatic or mild disease, provides a reason for optimism regarding the capacity of vaccination, prior infection, and/or both, to limit disease severity and transmission of variants of concern as they continue to arise and circulate.” |
| 60) Exposure to SARS-CoV-2 generates T-cell memory in the absence of a detectable viral infection, Wang, 2021 | “T-cell immunity is important for recovery from COVID-19 and provides heightened immunity for re-infection. However, little is known about the SARS-CoV-2-specific T-cell immunity in virus-exposed individuals…report virus-specific CD4+ and CD8+ T-cell memory in recovered COVID-19 patients and close contacts…close contacts are able to gain T-cell immunity against SARS-CoV-2 despite lacking a detectable infection.” |
| 61) CD8+ T-Cell Responses in COVID-19 Convalescent Individuals Target Conserved Epitopes From Multiple Prominent SARS-CoV-2 Circulating Variants, Redd, 2021and Lee, 2021 | “The CD4 and CD8 responses generated after natural infection are equally robust, showing activity against multiple “epitopes” (little segments) of the spike protein of the virus. For instance, CD8 cells responds to 52 epitopes and CD4 cells respond to 57 epitopes across the spike protein, so that a few mutations in the variants cannot knock out such a robust and in-breadth T cell response…only 1 mutation found in Beta variant-spike overlapped with a previously identified epitope (1/52), suggesting that virtually all anti-SARS-CoV-2 CD8+ T-cell responses should recognize these newly described variants.” |
| 62) Exposure to common cold coronaviruses can teach the immune system to recognize SARS-CoV-2,La Jolla, Crotty and Sette, 2020 | “Exposure to common cold coronaviruses can teach the immune system to recognize SARS-CoV-2” |
| 63) Selective and cross-reactive SARS-CoV-2 T cell epitopes in unexposed humans, Mateus, 2020 | “Found that the pre-existing reactivity against SARS-CoV-2 comes from memory T cells and that cross-reactive T cells can specifically recognize a SARS-CoV-2 epitope as well as the homologous epitope from a common cold coronavirus. These findings underline the importance of determining the impacts of pre-existing immune memory in COVID-19 disease severity.” |
| 64) Longitudinal observation of antibody responses for 14 months after SARS-CoV-2 infection, Dehgani-Mobaraki, 2021 | “Better understanding of antibody responses against SARS-CoV-2 after natural infection might provide valuable insights into the future implementation of vaccination policies. Longitudinal analysis of IgG antibody titers was carried out in 32 recovered COVID-19 patients based in the Umbria region of Italy for 14 months after Mild and Moderately-Severe infection…study findings are consistent with recent studies reporting antibody persistency suggesting that induced SARS-CoV-2 immunity through natural infection, might be very efficacious against re-infection (>90%) and could persist for more than six months. Our study followed up patients up to 14 months demonstrating the presence of anti-S-RBD IgG in 96.8% of recovered COVID-19 subjects.” |
| 65) Humoral and circulating follicular helper T cell responses in recovered patients with COVID-19, Juno, 2020 | “Characterized humoral and circulating follicular helper T cell (cTFH) immunity against spike in recovered patients with coronavirus disease 2019 (COVID-19). We found that S-specific antibodies, memory B cells and cTFH are consistently elicited after SARS-CoV-2 infection, demarking robust humoral immunity and positively associated with plasma neutralizing activity.” |
| 66) Convergent antibody responses to SARS-CoV-2 in convalescent individuals, Robbiani, 2020 | “149 COVID-19-convalescent individuals…antibody sequencing revealed the expansion of clones of RBD-specific memory B cells that expressed closely related antibodies in different individuals. Despite low plasma titres, antibodies to three distinct epitopes on the RBD neutralized the virus with half-maximal inhibitory concentrations (IC50 values) as low as 2 ng ml−1.” |
| 67) Rapid generation of durable B cell memory to SARS-CoV-2 spike and nucleocapsid proteins in COVID-19 and convalescence, Hartley, 2020 | “COVID-19 patients rapidly generate B cell memory to both the spike and nucleocapsid antigens following SARS-CoV-2 infection…RBD- and NCP-specific IgG and Bmem cells were detected in all 25 patients with a history of COVID-19.” |
| 68) Had COVID? You’ll probably make antibodies for a lifetime, Callaway, 2021 | “People who recover from mild COVID-19 have bone-marrow cells that can churn out antibodies for decades…the study provides evidence that immunity triggered by SARS-CoV-2 infection will be extraordinarily long-lasting.” |
| 69) A majority of uninfected adults show preexisting antibody reactivity against SARS-CoV-2, Majdoubi, 2021 | In greater Vancouver Canada, “using a highly sensitive multiplex assay and positive/negative thresholds established in infants in whom maternal antibodies have waned, we determined that more than 90% of uninfected adults showed antibody reactivity against the spike protein, receptor-binding domain (RBD), N-terminal domain (NTD), or the nucleocapsid (N) protein from SARS-CoV-2.” |
| 70) SARS-CoV-2-reactive T cells in healthy donors and patients with COVID-19, Braun, 2020 | “The results indicate that spike-protein cross-reactive T cells are present, which were probably generated during previous encounters with endemic coronaviruses.” |
| 71) Naturally enhanced neutralizing breadth against SARS-CoV-2 one year after infection, Wang, 2021 | “A cohort of 63 individuals who have recovered from COVID-19 assessed at 1.3, 6.2 and 12 months after SARS-CoV-2 infection…the data suggest that immunity in convalescent individuals will be very long lasting.” |
| 72) One Year after Mild COVID-19: The Majority of Patients Maintain Specific Immunity, But One in Four Still Suffer from Long-Term Symptoms, Rank, 2021 | “Long-lasting immunological memory against SARS-CoV-2 after mild COVID-19.” |
| 73) IDSA, 2021 | “Immune responses to SARS-CoV-2 following natural infection can persist for at least 11 months… natural infection (as determined by a prior positive antibody or PCR-test result) can confer protection against SARS-CoV-2 infection.” |
| 74) Assessment of protection against reinfection with SARS-CoV-2 among 4 million PCR-tested individuals in Denmark in 2020: a population-level observational study, Holm Hansen, 2021 | Denmark, “during the first surge (ie, before June, 2020), 533 381 people were tested, of whom 11 727 (2·20%) were PCR positive, and 525 339 were eligible for follow-up in the second surge, of whom 11 068 (2·11%) had tested positive during the first surge. Among eligible PCR-positive individuals from the first surge of the epidemic, 72 (0·65% [95% CI 0·51–0·82]) tested positive again during the second surge compared with 16 819 (3·27% [3·22–3·32]) of 514 271 who tested negative during the first surge (adjusted RR 0·195 [95% CI 0·155–0·246]).” |
| 75) Antigen-Specific Adaptive Immunity to SARS-CoV-2 in Acute COVID-19 and Associations with Age and Disease Severity, Moderbacher, 2020 | “Adaptive immune responses limit COVID-19 disease severity…multiple coordinated arms of adaptive immunity control better than partial responses…completed a combined examination of all three branches of adaptive immunity at the level of SARS-CoV-2-specific CD4+ and CD8+ T cell and neutralizing antibody responses in acute and convalescent subjects. SARS-CoV-2-specific CD4+ and CD8+ T cells were each associated with milder disease. Coordinated SARS-CoV-2-specific adaptive immune responses were associated with milder disease, suggesting roles for both CD4+ and CD8+ T cells in protective immunity in COVID-19.” |
| 76) Detection of SARS-CoV-2-Specific Humoral and Cellular Immunity in COVID-19 Convalescent Individuals, Ni, 2020 | “Collected blood from COVID-19 patients who have recently become virus-free, and therefore were discharged, and detected SARS-CoV-2-specific humoral and cellular immunity in eight newly discharged patients. Follow-up analysis on another cohort of six patients 2 weeks post discharge also revealed high titers of immunoglobulin G (IgG) antibodies. In all 14 patients tested, 13 displayed serum-neutralizing activities in a pseudotype entry assay. Notably, there was a strong correlation between neutralization antibody titers and the numbers of virus-specific T cells.” |
| 77) Robust SARS-CoV-2-specific T-cell immunity is maintained at 6 months following primary infection, Zuo, 2020 | “Analysed the magnitude and phenotype of the SARS-CoV-2 cellular immune response in 100 donors at six months following primary infection and related this to the profile of antibody level against spike, nucleoprotein and RBD over the previous six months. T-cell immune responses to SARS-CoV-2 were present by ELISPOT and/or ICS analysis in all donors and are characterised by predominant CD4+ T cell responses with strong IL-2 cytokine expression… functional SARS-CoV-2-specific T-cell responses are retained at six months following infection.” |
| 78) Negligible impact of SARS-CoV-2 variants on CD4+ and CD8+ T cell reactivity in COVID-19 exposed donors and vaccinees, Tarke, 2021 | “Performed a comprehensive analysis of SARS-CoV-2-specific CD4+ and CD8+ T cell responses from COVID-19 convalescent subjects recognizing the ancestral strain, compared to variant lineages B.1.1.7, B.1.351, P.1, and CAL.20C as well as recipients of the Moderna (mRNA-1273) or Pfizer/BioNTech (BNT162b2) COVID-19 vaccines… the sequences of the vast majority of SARS-CoV-2 T cell epitopes are not affected by the mutations found in the variants analyzed. Overall, the results demonstrate that CD4+ and CD8+ T cell responses in convalescent COVID-19 subjects or COVID-19 mRNA vaccinees are not substantially affected by mutations.” |
| 79) A 1 to 1000 SARS-CoV-2 reinfection proportion in members of a large healthcare provider in Israel: a preliminary report, Perez, 2021 | Israel, “out of 149,735 individuals with a documented positive PCR test between March 2020 and January 2021, 154 had two positive PCR tests at least 100 days apart, reflecting a reinfection proportion of 1 per 1000.” |
| 80) Persistence and decay of human antibody responses to the receptor binding domain of SARS-CoV-2 spike protein in COVID-19 patients, Iyer, 2020 | “Measured plasma and/or serum antibody responses to the receptor-binding domain (RBD) of the spike (S) protein of SARS-CoV-2 in 343 North American patients infected with SARS-CoV-2 (of which 93% required hospitalization) up to 122 days after symptom onset and compared them to responses in 1548 individuals whose blood samples were obtained prior to the pandemic…IgG antibodies persisted at detectable levels in patients beyond 90 days after symptom onset, and seroreversion was only observed in a small percentage of individuals. The concentration of these anti-RBD IgG antibodies was also highly correlated with pseudovirus NAb titers, which also demonstrated minimal decay. The observation that IgG and neutralizing antibody responses persist is encouraging, and suggests the development of robust systemic immune memory in individuals with severe infection.” |
| 81) A population-based analysis of the longevity of SARS-CoV-2 antibody seropositivity in the United States, Alfego, 2021 | “To track population-based SARS-CoV-2 antibody seropositivity duration across the United States using observational data from a national clinical laboratory registry of patients tested by nucleic acid amplification (NAAT) and serologic assays… specimens from 39,086 individuals with confirmed positive COVID-19…both S and N SARS-CoV-2 antibody results offer an encouraging view of how long humans may have protective antibodies against COVID-19, with curve smoothing showing population seropositivity reaching 90% within three weeks, regardless of whether the assay detects N or S-antibodies. Most importantly, this level of seropositivity was sustained with little decay through ten months after initial positive PCR.” |
| 82) What are the roles of antibodies versus a durable, high- quality T-cell response in protective immunity against SARS-CoV-2? Hellerstein, 2020 | “Progress in laboratory markers for SARS-CoV2 has been made with identification of epitopes on CD4 and CD8 T-cells in convalescent blood. These are much less dominated by spike protein than in previous coronavirus infections. Although most vaccine candidates are focusing on spike protein as antigen, natural infection by SARS-CoV-2 induces broad epitope coverage, cross-reactive with other betacoronviruses.” |
| 83) Broad and strong memory CD4+ and CD8+ T cells induced by SARS-CoV-2 in UK convalescent COVID-19 patients, Peng, 2020 | “Study of 42 patients following recovery from COVID-19, including 28 mild and 14 severe cases, comparing their T cell responses to those of 16 control donors…found the breadth, magnitude and frequency of memory T cell responses from COVID-19 were significantly higher in severe compared to mild COVID-19 cases, and this effect was most marked in response to spike, membrane, and ORF3a proteins…total and spike-specific T cell responses correlated with the anti-Spike, anti-Receptor Binding Domain (RBD) as well as anti-Nucleoprotein (NP) endpoint antibody titre…furthermore showed a higher ratio of SARS-CoV-2-specific CD8+ to CD4+ T cell responses…immunodominant epitope clusters and peptides containing T cell epitopes identified in this study will provide critical tools to study the role of virus-specific T cells in control and resolution of SARS-CoV-2 infections.” |
| 84) Robust T Cell Immunity in Convalescent Individuals with Asymptomatic or Mild COVID-19, Sekine, 2020 | “SARS-CoV-2-specific memory T cells will likely prove critical for long-term immune protection against COVID-19…mapped the functional and phenotypic landscape of SARS-CoV-2-specific T cell responses in unexposed individuals, exposed family members, and individuals with acute or convalescent COVID-19…collective dataset shows that SARS-CoV-2 elicits broadly directed and functionally replete memory T cell responses, suggesting that natural exposure or infection may prevent recurrent episodes of severe COVID-19.” |
| 85) Potent SARS-CoV-2-Specific T Cell Immunity and Low Anaphylatoxin Levels Correlate With Mild Disease Progression in COVID-19 Patients, Lafron, 2021 | “Provide a full picture of cellular and humoral immune responses of COVID-19 patients and prove that robust polyfunctional CD8+ T cell responses concomitant with low anaphylatoxin levels correlate with mild infections.” |
| 86) SARS-CoV-2 T-cell epitopes define heterologous and COVID-19 induced T-cell recognition, Nelde, 2020 | “The first work identifying and characterizing SARS-CoV-2-specific and cross-reactive HLA class I and HLA-DR T-cell epitopes in SARS-CoV-2 convalescents (n = 180) as well as unexposed individuals (n = 185) and confirming their relevance for immunity and COVID-19 disease course…cross-reactive SARS-CoV-2 T-cell epitopes revealed pre-existing T-cell responses in 81% of unexposed individuals, and validation of similarity to common cold human coronaviruses provided a functional basis for postulated heterologous immunity in SARS-CoV-2 infection…intensity of T-cell responses and recognition rate of T-cell epitopes was significantly higher in the convalescent donors compared to unexposed individuals, suggesting that not only expansion, but also diversity spread of SARS-CoV-2 T-cell responses occur upon active infection.” |
| 87) Karl Friston: up to 80% not even susceptible to Covid-19, Sayers, 2020 | “Results have just been published of a study suggesting that 40%-60% of people who have not been exposed to coronavirus have resistance at the T-cell level from other similar coronaviruses like the common cold…the true portion of people who are not even susceptible to Covid-19 may be as high as 80%.” |
| 88) CD8+ T cells specific for an immunodominant SARS-CoV-2 nucleocapsid epitope cross-react with selective seasonal coronaviruses, Lineburg, 2021 | “Screening of SARS-CoV-2 peptide pools revealed that the nucleocapsid (N) protein induced an immunodominant response in HLA-B7+ COVID-19-recovered individuals that was also detectable in unexposed donors…the basis of selective T cell cross-reactivity for an immunodominant SARS-CoV-2 epitope and its homologs from seasonal coronaviruses, suggesting long-lasting protective immunity.” |
| 89) SARS-CoV-2 genome-wide mapping of CD8 T cell recognition reveals strong immunodominance and substantial CD8 T cell activation in COVID-19 patients, Saini, 2020 | “COVID-19 patients showed strong T cell responses, with up to 25% of all CD8+ lymphocytes specific to SARS-CoV-2-derived immunodominant epitopes, derived from ORF1 (open reading frame 1), ORF3, and Nucleocapsid (N) protein. A strong signature of T cell activation was observed in COVID-19 patients, while no T cell activation was seen in the ‘non-exposed’ and ‘high exposure risk’ healthy donors.” |
| 90) Equivalency of Protection from Natural Immunity in COVID-19 Recovered Versus Fully Vaccinated Persons: A Systematic Review and Pooled Analysis, Shenai, 2021 | “Systematic review and pooled analysis of clinical studies to date, that (1) specifically compare the protection of natural immunity in the COVID-recovered versus the efficacy of full vaccination in the COVID-naive, and (2) the added benefit of vaccination in the COVID-recovered, for prevention of subsequent SARS-CoV-2 infection…review demonstrates that natural immunity in COVID-recovered individuals is, at least, equivalent to the protection afforded by full vaccination of COVID-naïve populations. There is a modest and incremental relative benefit to vaccination in COVID-recovered individuals; however, the net benefit is marginal on an absolute basis.” |
| 91) ChAdOx1nCoV-19 effectiveness during an unprecedented surge in SARS CoV-2 infections, Satwik, 2021 | “The third key finding is that previous infections with SARS-CoV-2 were significantly protective against all studied outcomes, with an effectiveness of 93% (87 to 96%) seen against symptomatic infections, 89% (57 to 97%) against moderate to severe disease and 85% (-9 to 98%) against supplemental oxygen therapy. All deaths occurred in previously uninfected individuals. This was higher protection than that offered by single or double dose vaccine.” |
| 92) SARS-CoV-2 specific T cells and antibodies in COVID-19 protection: a prospective study, Molodtsov, 2021 |
“Explore the impact of T cells and to quantify the protective levels of the immune responses…5,340 Moscow residents were evaluated for the antibody and cellular immune responses to SARS-CoV-2 and monitored for COVID-19 up to 300 days. The antibody and cellular responses were tightly interconnected, their magnitude inversely correlated with infection probability. Similar maximal level of protection was reached by individuals positive for both types of responses and by individuals with antibodies alone…T cells in the absence of antibodies provided an intermediate level of protection.” |
| 93) Negligible impact of SARS-CoV-2 variants on CD4+ and CD8+ T cell reactivity in COVID-19 exposed donors and vaccinees, Tarke, 2021 | “Demonstrate that the sequences of the vast majority of SARS-CoV-2 T cell epitopes are not affected by the mutations found in the variants analyzed. Overall, the results demonstrate that CD4+ and CD8+ T cell responses in convalescent COVID-19 subjects or COVID-19 mRNA vaccinees are not substantially affected by mutations found in the SARS-CoV-2 variants.” |
| 94) Anti- SARS-CoV-2 Receptor Binding Domain Antibody Evolution after mRNA Vaccination, Cho, 2021 | “SARS-CoV-2 infection produces B-cell responses that continue to evolve for at least one year. During that time, memory B cells express increasingly broad and potent antibodies that are resistant to mutations found in variants of concern.” |
| 95) Seven-month kinetics of SARS-CoV-2 antibodies and role of pre-existing antibodies to human coronaviruses, Ortega, 2021 | “Impact of pre-existing antibodies to human coronaviruses causing common cold (HCoVs), is essential to understand protective immunity to COVID-19 and devise effective surveillance strategies…after the peak response, anti-spike antibody levels increase from ~150 days post-symptom onset in all individuals (73% for IgG), in the absence of any evidence of re-exposure. IgG and IgA to HCoV are significantly higher in asymptomatic than symptomatic seropositive individuals. Thus, pre-existing cross-reactive HCoVs antibodies could have a protective effect against SARS-CoV-2 infection and COVID-19 disease.” |
| 96) Immunodominant T-cell epitopes from the SARS-CoV-2 spike antigen reveal robust pre-existing T-cell immunity in unexposed individuals, Mahajan, 2021 | “Findings suggest that SARS-CoV-2 reactive T-cells are likely to be present in many individuals because of prior exposure to flu and CMV viruses.” |
| 97) Detection of SARS-CoV-2-Specific Humoral and Cellular Immunity in COVID-19 Convalescent Individuals, Ni, 2020 | “Collected blood from COVID-19 patients who have recently become virus-free, and therefore were discharged, and detected SARS-CoV-2-specific humoral and cellular immunity in eight newly discharged patients… In all 14 patients tested, 13 displayed serum-neutralizing activities in a pseudotype entry assay. Notably, there was a strong correlation between neutralization antibody titers and the numbers of virus-specific T cells.” |
| 98) Neutralizing Antibody Responses to Severe Acute Respiratory Syndrome Coronavirus 2 in Coronavirus Disease 2019 Inpatients and Convalescent Patients, Wang, 2020 | “117 blood samples were collected from 70 COVID-19 inpatients and convalescent patients…the neutralizing antibodies were detected even at the early stage of disease, and a significant response was shown in convalescent patients.” |
| 99) Not just antibodies: B cells and T cells mediate immunity to COVID-19, Cox, 2020 | “Reports that antibodies to SARS-CoV-2 are not maintained in the serum following recovery from the virus have caused alarm…the absence of specific antibodies in the serum does not necessarily mean an absence of immune memory.” |
| 100) T cell immunity to SARS-CoV-2 following natural infection and vaccination, DiPiazza, 2020 | “Although T cell durability to SARS-CoV-2 remains to be determined, current data and past experience from human infection with other CoVs demonstrate the potential for persistence and the capacity to control viral replication and host disease, and importance in vaccine-induced protection.” |
| 101) Durable SARS-CoV-2 B cell immunity after mild or severe disease, Ogega, 2021 | “Multiple studies have shown loss of severe acute respiratory syndrome coronavirus 2-specific (SARS-CoV-2-specific) antibodies over time after infection, raising concern that humoral immunity against the virus is not durable. If immunity wanes quickly, millions of people may be at risk for reinfection after recovery from coronavirus disease 2019 (COVID-19). However, memory B cells (MBCs) could provide durable humoral immunity even if serum neutralizing antibody titers decline… data indicate that most SARS-CoV-2-infected individuals develop S-RBD-specific, class-switched rMBCs that resemble germinal center-derived B cells induced by effective vaccination against other pathogens, providing evidence for durable B cell-mediated immunity against SARS-CoV-2 after mild or severe disease.” |
| 102) Memory T cell responses targeting the SARS coronavirus persist up to 11 years post-infection., Ng, 2016 | “All memory T cell responses detected target the SARS-Co-V structural proteins… these responses were found to persist up to 11 years post-infection… knowledge of the persistence of SARS-specific celullar immunity targeting the viral structural proteins in SARS-recovered individuals is important.” |
Natural Immunity articles
| 11810 |  August 5, 2021
August 5, 2021
|
Covid Outbreak Hits Carnival Cruise Despite Every Guest and Staff Member Being ‘Vaccinated’ |
| 11590 |  August 5, 2021
August 5, 2021
|
Vaccine Adverse Events in the US VAERS System |
| 11392 |  August 5, 2021
August 5, 2021
|
Rand Paul Calls NIH Director “Stupid” After Call To Wear Masks At Home |
| 10677 |  August 4, 2021
August 4, 2021
|
The Awareness Foundation Covid 19 Roundtable |
| 10381 |  August 3, 2021
August 3, 2021
|
Australia – Vaccinated STILL GOT INFECTED |
| 18909 | August 3, 2021 | COVID-19 in Iceland: Vaccination Has Not Led to Herd Immunity, Says Chief Epidemiologist |
| 13128 | August 3, 2021 | My own country of Canada just kicked me out because my Covid immunity was acquired naturally and not from a vaccine |
| 8628 |  July 31, 2021
July 31, 2021
|
Dr. Robert Malone (mRNA vaccine inventor) – Steven Bannon War Room |
| 7993 |  July 31, 2021
July 31, 2021
|
COVID Vaccine Not As Effective As We’re Told, Masks Forever, Fauci is a Liar, Alex Berenson |
| 7893 | July 31, 2021 | Reports of Serious Injuries After Vaccines Surge as CDC Says Vaccinated May Be as Likely to Spread COVID as Unvaxxed |