mRNA Covid-19 Vaccines in Pregnant Women
List of authors.
- Laura E. Riley, M.D.
After Emergency Use Authorization was granted for the messenger RNA (mRNA) vaccines BNT162b2 (Pfizer–BioNTech) and mRNA-1273 (Moderna), persons at the highest risk for coronavirus disease 2019 (Covid-19)–related illness and death were prioritized for vaccination.1 Among these were pregnant women, yet they had been excluded from initial vaccine trials. Pregnant women and their clinicians were left to weigh the documented risks of Covid-19 infection against the unknown safety risks of vaccination in deciding whether to receive the vaccine.
Before the vaccine rollout, multiple cohort studies documented that pregnant women were at greater risk than nonpregnant women for severe disease after Covid-19 infection, resulting in intensive care unit admission, mechanical ventilation, and death.2,3 Pregnant women with coexisting illnesses such as diabetes, hypertension, and obesity were recognized to be at even greater risk.4 Studies also showed an increased risk of pregnancy complications — including preterm birth, cesarean delivery, and preeclampsia — associated with Covid-19 infection during pregnancy.5 Therefore, clinicians relied on developmental and reproductive animal data from Moderna that showed no safety concerns, and there was no biologically plausible reason that the mRNA technology would be harmful in pregnancy. Pregnant women were counseled to consider the available evidence and make personal decisions about vaccination in the absence of human safety data.
In this issue of the Journal, Shimabukuro et al.6 provide much-needed preliminary data on the safety of these vaccines in pregnancy on the basis of the v-safe surveillance system and pregnancy registry. V-safe, a new smartphone-based surveillance system from the Centers for Disease Control and Prevention that is available to all Covid-19 vaccine recipients, sends text messages to assess general health and pregnancy status during a period of 12 months after vaccination. Persons who identify as pregnant can enroll in the v-safe pregnancy registry, which contacts participants by telephone to answer in-depth questions.
The report by Shimabukuro et al. includes safety results for 35,691 v-safe participants 16 to 54 years of age who identified as pregnant and the first 3958 participants who enrolled in the v-safe pregnancy registry. In both cohorts, 54% of the participants received the Pfizer–BioNTech vaccine and 46% received the Moderna vaccine. The age distribution, status with respect to race and ethnic group, and timing of the first dose were similar with each vaccine. Among v-safe participants, 86.5% had a known pregnancy at the time of vaccination, and 13.5% reported a positive pregnancy test after vaccination. Among v-safe pregnancy registry participants, 28.6% received vaccine in the first trimester, 43.3% in the second trimester, and 25.7% in the third trimester.
Among 827 registry participants who reported a completed pregnancy, 104 experienced spontaneous abortions and 1 had a stillbirth. A total of 712 pregnancies (86.1%) resulted in a live birth, mostly among participants who received their first vaccination dose in the third trimester. Among live-born infants, the incidences of preterm birth (9.4%), small size for gestational age (3.2%), and congenital anomalies (2.2%) were consistent with those expected on the basis of published literature. There were no neonatal deaths. These are reassuring data based on reports from pregnant women mostly vaccinated in the third trimester.
In addition, rates of local and systemic reactions after vaccination among v-safe participants who identified as pregnant were similar to those in a larger group of nonpregnant women, which suggests that the physiologic changes in pregnancy do not materially affect such reactions. The most common side effect was injection-site pain, with fatigue, headache, and myalgia reported substantially more often after the second dose. Fever was reported in a small number of people after the first dose and in approximately a third of recipients after the second dose.
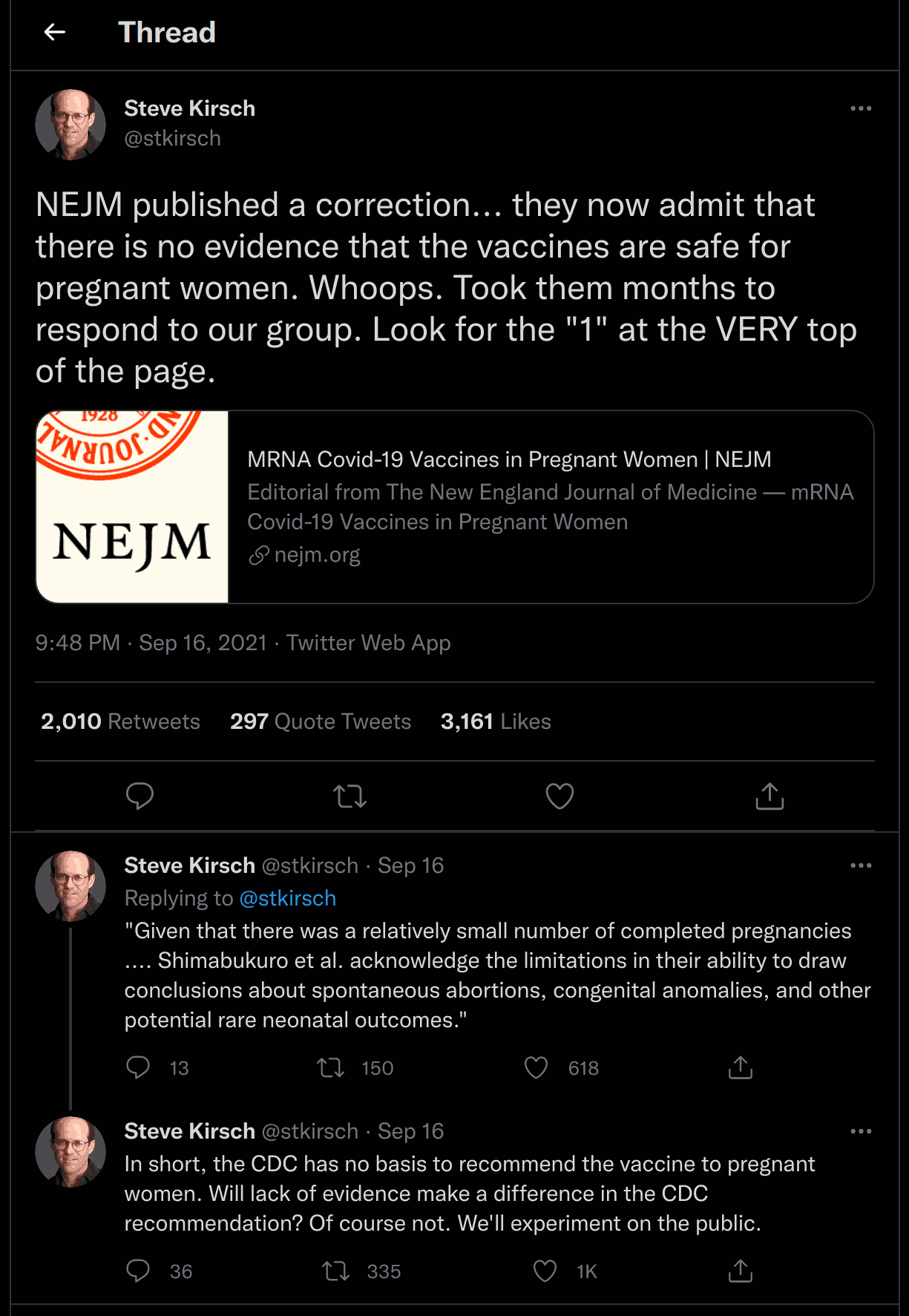
Given that there was a relatively small number of completed pregnancies and that live births were typically after vaccination in the third trimester, Shimabukuro et al. acknowledge the limitations in their ability to draw conclusions about spontaneous abortions, congenital anomalies, and other potential rare neonatal outcomes. Despite these limitations, this report provides important information that was not previously available.
With the pandemic ongoing and pregnant women at high risk for serious illness if infected with Covid-19, vaccination is a critical prevention strategy. The dearth of safety information about pregnancy, which existed at a time when thousands of pregnant women were grappling with decisions about vaccination, highlights the importance of recent efforts to enroll pregnant women in trials, including ongoing vaccine trials; a trial is currently under way to study the effects of the BNT162b2 vaccine in pregnant women and their infants (ClinicalTrials.gov number, NCT04754594. opens in new tab).
It is notable that as of April 26, 2021, more than 100,000 pregnant women reported having received a Covid-19 vaccination and yet only a small fraction (4.7%) have enrolled in the v-safe pregnancy registry.7 This situation underscores the urgent need not only to include pregnant women in clinical trials, but also to invest in public health surveillance systems for pregnancy, involving much larger numbers of women. To prepare for the next pandemic and improve health outcomes for pregnant women more generally, it is past time to invest in maternal health surveillance and research.
Disclosure forms provided by the author are available with the full text of this editorial at NEJM.org.
This editorial was updated on September 8, 2021, at NEJM.org.
Author Affiliations
From New York–Presbyterian/Weill Cornell Medical Center and Weill Cornell Medicine, New York.
Supplementary Material
| Disclosure Forms | 146KB |
References (7)
-
1.
-
2.
-
3.
-
4.
-
5.
-
6.
Citing Article (1)