Photobiomodulation Improves Serum Cytokine Response in Mild to Moderate COVID-19: The First Randomized, Double-Blind, Placebo Controlled, Pilot Study
- 1Chronic Respiratory Diseases Research Center, National Research Institute of Tuberculosis and Lung Diseases, Shahid Beheshti University of Medical Sciences, Tehran, Iran
- 2Department of Immunology, School of Public Health, University of Medical Sciences, Tehran, Iran
- 3National Research Institute of Tuberculosis and Lung Diseases (NRITLD), Shahid Beheshti University of Medical Sciences, Tehran, Iran
- 4Medical Research & Innovation Department, Medical and Biomedical Consultancy Office “Innolys”, Illkirch-Graffenstaden, France
Background: Because the major event in COVID-19 is the release of pre- and inflammatory cytokines, finding a reliable therapeutic strategy to inhibit this release, help patients manage organ damage and avoid ICU admission or severe disease progression is of paramount importance. Photobiomodulation (PBM), based on numerous studies, may help in this regard, and the present study sought to evaluate the effects of said technology on cytokine reduction.
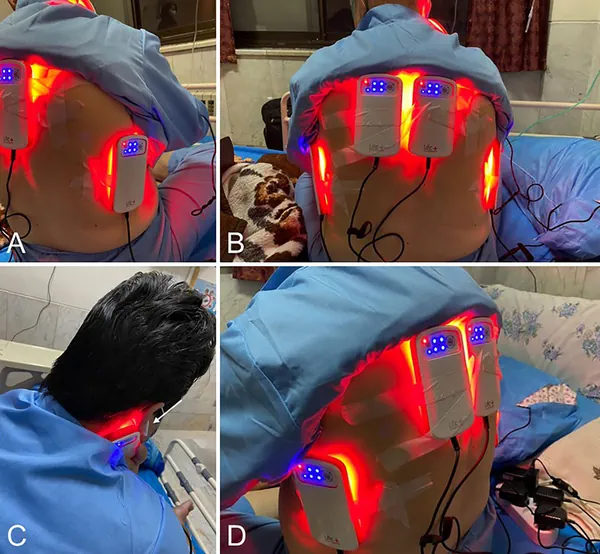
Methods: This study was conducted in the 2nd half of 2021. The current study included 52 mild-to-moderately ill COVID-19, hospitalized patients. They were divided in two groups: a Placebo group and a PBM group, treated with PBM (620-635 nm light via 8 LEDs that provide an energy density of 45.40 J/cm2 and a power density of 0.12 W/cm2), twice daily for three days, along with classical approved treatment. 28 patients were in Placebo group and 24 in PBM group. In both groups, blood samples were taken four times in three days and serum IL-6, IL-8, IL-10, and TNF-α levels were determined.
Results: During the study period, in PBM group, there was a significant decrease in serum levels of IL-6 (-82.5% +/- 4, P<0.001), IL-8 (-54.4% ± 8, P<0.001), and TNF-α (-82.4% ± 8, P<0.001), although we did not detect a significant change in IL-10 during the study. The IL-6/IL-10 Ratio also improved in PBM group. The Placebo group showed no decrease or even an increase in these parameters. There were no reported complications or sequelae due to PBM therapy throughout the study.
Conclusion: The major cytokines in COVID-19 pathophysiology, including IL-6, IL-8, and TNF-α, responded positively to PBM therapy and opened a new window for inhibiting and managing a cytokine storm within only 3-10 days.
Introduction
COVID-19 is one of the most – if not the most – challenging pandemics in the modern world. It is caused by the SARS-CoV 2 coronavirus (1) and triggers severe acute respiratory syndrome (SARS). This condition is associated with overexpression of inflammatory markers such as interleukins (2).
Basically, there are two known phases of the immune response against COVID-19 in the body (3). The first phase belongs to B/T cell immunity and leads to the release of immunoglobulins (IgM and IgG) in the body. This is usually effective against a broad spectrum of infections, including bacterial, viral and fungal infections. The second phase, which is much more crucial in COVID-19 because it is an intracellular viral infection, results in the secretion of a variety of cytokines into the bloodstream by T cells and macrophages, of which IL1-β, IL-2, IL-8, IL-10, IL-6, IL-12, IFN-γ, and TNF-α are the best known (4, 5).
This second phase can be dramatically dysregulated in patients – sometimes referred to as a “cytokine storm” – leading to multiple organ failure, thromboembolism, and death (6). This is at least part of the explanation for the high mortality rate in COVID-19.
It is likely that the use of immunomodulatory agents could be a promising therapeutic strategy to reduce or even prevent this dysregulation and improve survival of moderate-to-severe patients by inhibiting or at least modulating the severe immune response to ARDS. Immunosuppressive drugs such as corticosteroids, a well-known group of immunomodulatory drugs, have been used along this pathway. However, their use may also increase the risk of secondary infections and prolongation of hospital stay (7, 8).
To date, there is no globally approved treatment for this “cytokine storm”. Therefore, there is an urgent need for new solutions. Here, we propose to test a non-drug approach to modulate the host immune response to improve the prognosis of patients.
According to previous studies, IL-6, IL-8, IL-10 and TNF-α seem to play an important role in the patient’s vital prognosis (9, 10). Therefore, in the present study, we focus on these 4. IL-6 is a pleiotropic cytokine that plays a crucial role in the pathophysiology of ARDS and leads to poor prognosis for patients (9). IL-8 is also involved in the pathophysiology of ARDS, neutrophil chemotaxis and lung tissue survival, and increases disease severity, resulting mortality in humans (10). IL-10 is mainly known as an anti-inflammatory cytokine, especially in chronic diseases such as (not conclusive) chronic obstructive pulmonary disease (COPD) (11), tuberculosis (12), rheumatoid arthritis (13), etc. IL-10 may actually modulate the production of inflammatory cytokines to reduce the risk of tissue damage (14–16). TNF-α is an important proinflammatory marker involved in several immune pathways, such as neutrophil adhesion and activation, but also in the production of IL-6 and in the development of edema due to coagulation in acute pneumonia (17, 18).
Photobiomodulation (PBM), also known as low-level light therapy (LLLT), has been studied and used for over 50 years (19–26) to protect cells from dying (22, 24, 27–30) and to target and treat inflammation in organs (31, 32). It consists of the application of a narrow spectral bandwidth light from red to near-infrared light (600-1000 nm wavelength) with a power density of 1-5000 mW/cm2 to modulate cell metabolism, signal transduction, and secretion in the body (33–35).
Since PBM has shown promising effects on inflammation control in many medical situations (15, 31, 36–40), such as ARDS in the lung (10), it seems to be an alternative approach of choice to address the need for immune regulation in moderate to severe COVID-19 patients (41).
De Lima et al. indicated that PBM effectively affects TNF-α reduction in alveolar macrophages to reduce the incidence of ARDS in mice (35). PBM has also been shown to inhibit the migration of neutrophils into lung tissue, resulting in less activation and higher apoptosis of these cells to reduce neutrophil accumulation and ultimately alleviate the severity of pneumonia and ARDS (10). Some studies have shown that PBM leads to a decrease in IL-6 in serum and lung tissue in COPD patients, while increasing the CD4+/CD8+ ratio (10, 42, 43), and decreasing the risk of fibrosis in chronic pneumonia (36).
Based on the above findings, the current study sought to investigate the clinical effects of PBM on mild and moderate COVID-19 cases hospitalized in a tertiary college referral center for respiratory and infectious diseases in Tehran.

 Seyed Mehran Marashian1,
Seyed Mehran Marashian1,  Florian Reinhart
Florian Reinhart