Researchers in “gold standard” collaboration struggle to find benefit from surgical over no masks, or N95 respirators over surgical. Findings buoy warnings by PPE expert that even “perfect rate of capture” by N95s can’t stop COVID transmission.
By
Updated: January 31, 2023 – 11:12pm
An international research collaboration that reviewed several dozen rigorous studies of “physical interventions” against influenza and COVID-19 through last year failed to find even a modest effect on infection or illness rates from masks of all qualities.
Published in the peer-reviewed Cochrane Database of Systematic Reviews, run by the British evidence-based medicine charity Cochrane, the study raises new doubts about ongoing mask mandates and public health recommendations worldwide.
The CDC is still recommending masking in areas with “high” transmission levels — fewer than 4% of U.S. counties — as well as indoor masking to protect high-risk contacts in “medium” counties (27%).
Masks are still required in educational institutions in Democratic strongholds such as New York, New Jersey, Massachusetts, Pennsylvania, Washington and California, according to the Daily Mail. Boston Public Schools denied its “temporary masking protocol” in early January was a “mandate,” following a public letter against the policy by student Enrique Abud Evereteze.
South Korea is still requiring masks on public transport and in medical facilities after dropping COVID mandates in most indoor settings, including gyms, Monday, Reuters reported.
The researchers for the Cochrane study are affiliated with a geographically disparate range of institutions in the U.K., Canada, Australia, Italy and Saudi Arabia. Half are affiliated with the Institute for Evidence-Based Healthcare at Australia’s Bond University. The corresponding author is the University of Calgary’s John Conly.
Unlisted author Carl Heneghan, director of the Centre for Evidence-Based Medicine at the University of Oxford, gave a brief summary of the study population and findings on Twitter.
Jefferson_et_al-2023-Cochrane_Database_of_Systematic_ReviewsWe included 11 new RCTs and cluster‐RCTs (610,872 participants) in this update, bringing the total number of RCTs to 78.
— Carl Heneghan (@carlheneghan) January 30, 2023
The team added 11 new randomized controlled trials and “cluster-RCTs,” which randomize groups of subjects rather than individuals, to its prior review from November 2020, for a total of 78 studies. The additions included COVID pandemic trials: two from Mexico and one each from England, Norway, Denmark and Bangladesh, the latter two well known internationally.
The Danish study had trouble finding a major journal willing to publish its controversial findings that wearing surgical masks had no statistically significant effect on infection rates, even among those who claimed to wear them “exactly as instructed.”
Mainstream media overlooked red flags in the Bangladeshi mask study, which found no effect for surgical masks under age 50 and a difference of only 20 infections between control and treatment groups among 342,000 adults.
Cochrane itself had a spat with Instagram in November 2021 over sharing purported COVID misinformation, even though the group does not accept “commercial or conflicted funding” and its funding partners include the U.S. National Institutes of Health and U.K. National Institute for Health and Care Research.
Cochrane reviews are the 'gold standard' in evidence-based medicine. They follow a rigorous methodology and only consider high quality evidence. As such, the review included a limited number of studies and has moderate power to detect small effects.
2/— Prof Francois Balloux (@BallouxFrancois) January 31, 2023
The updated Cochrane review included 10 cluster RCTs in the “community” and two with healthcare workers totalling about 290,000 participants, comparing the effect of surgical versus no masks.
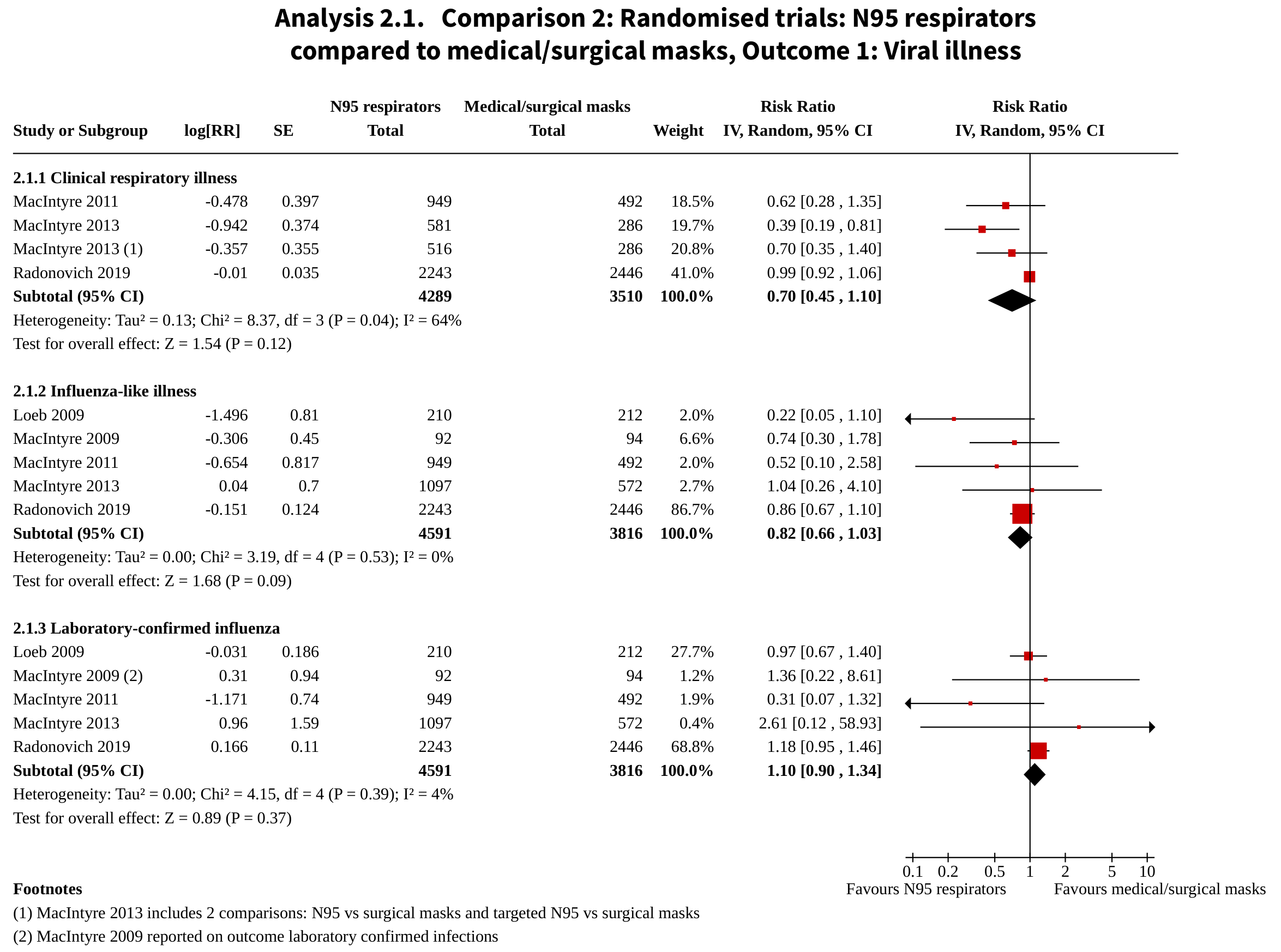
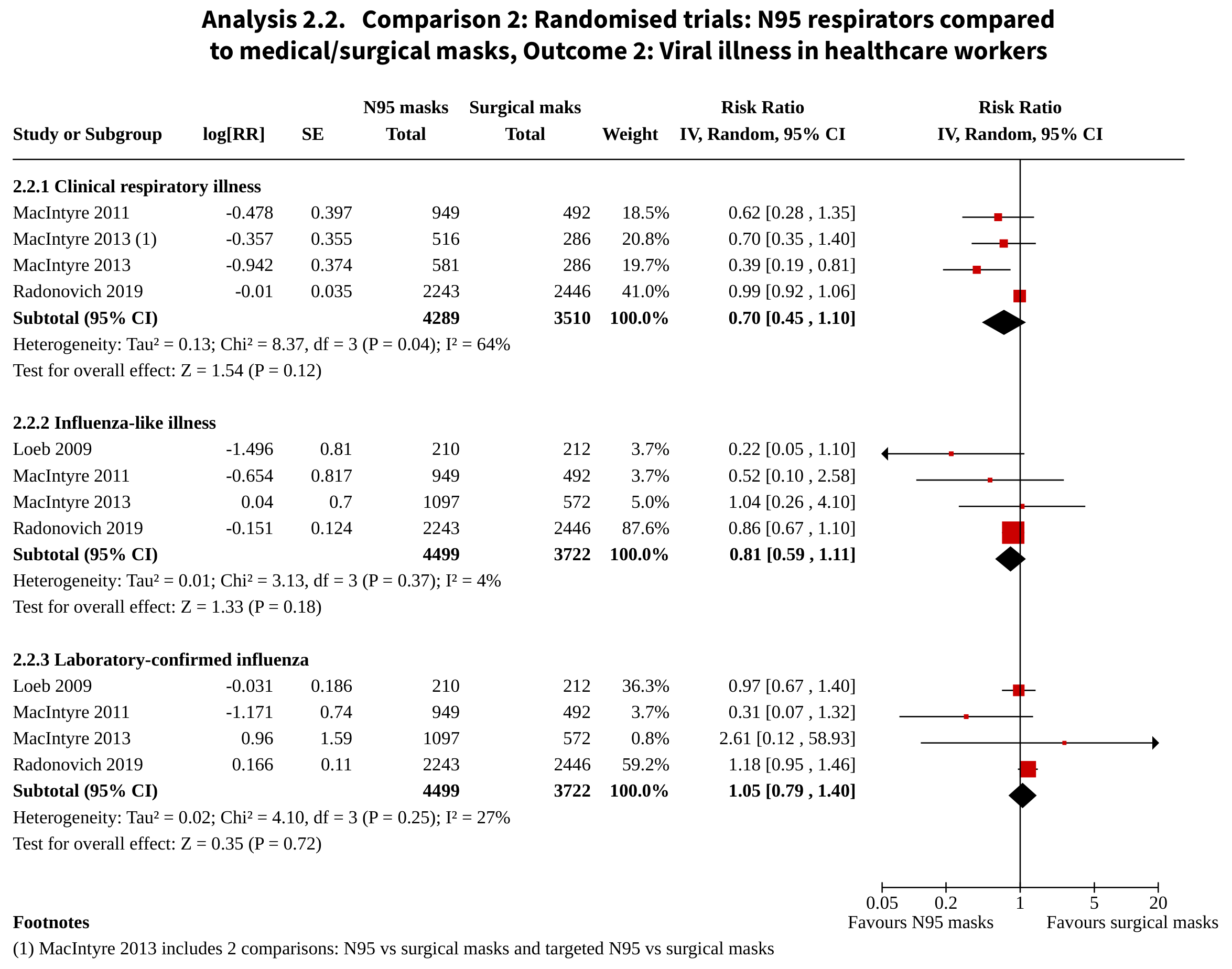
They measured risk ratios, which below 1 means the intervention improved the outcome and above 1 worsened it. The closer to 1, the less effect it had.
In the community, mask-wearing “probably makes little to no difference” in either influenza-like or COVID-like illness (0.95) or “laboratory-confirmed” infections of either virus (1.01). While the confirmed-infections finding had a much wider confidence interval, the team called both these results “moderate-certainty evidence.”
Researchers had more trouble determining the effect of respirators such as N95s — which the CDC only recommended two years into the pandemic — versus surgical masks. Five studies (four healthcare and one household), with a total of 16,000 participants, found a risk ratio of 0.70 for “clinical respiratory illness” but deemed it “very low-certainty evidence,” with a wide confidence interval. The RR was 0.82 for influenza-like illness, deemed “low-certainty” with a smaller confidence interval.
They were more confident in results for respirators versus surgical masks on lab-confirmed influenza: RR of 1.10 among the 8,400 participants in those trials, and no difference when the household trial was excluded.
2/ LARGE Cochrane Rev (just published 1/30/23) of RCT data ALSO CONFIRMS NO BENEFIT of N95 masks vs. med/surg masks, in either community (n~8K) or HCW (n~8K) settings for prevention of flu-like illness or lab confirmed flu https://t.co/N4TkgI4uUR pic.twitter.com/0DCdYAPo7x
— Andrew Bostom, MD, MS (@andrewbostom) January 31, 2023
Former White House COVID adviser Michael Osterholm tried to discredit one of the studies in the respiratory-surgical review, led by researchers at Canada’s McMaster University, when it was published in December in the Annals of Internal Medicine.
An expert on personal protective equipment and regulatory compliance, who warned colleges nearly two years ago their mask mandates violated disability integration law, told Just the News she has reviewed many of the RCTs the Cochrane team studied.
Megan Mansell said she expects to keep seeing “unreasonable responses when a decent RCT is published.” She cited her interactions with critics of the McMaster study, whose “primary complaint is that the individuals weren’t monitored for N95 compliance 24/7, which is both outside of the terms of safe wear for the apparatus and wholly unreasonable.”
Mansell wrote a lengthy and somewhat technical essay last week explaining why even “a perfect rate of capture” by N95s still provides “plentiful enough potential exposure” for infection, based on “severity of illness, immune response of a given individual, and progress in the course of illness.”
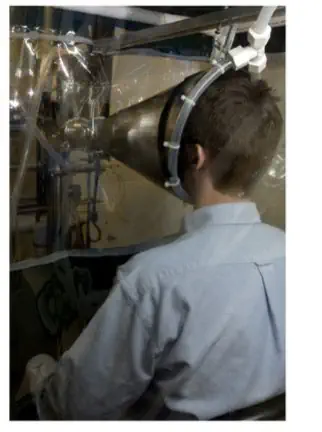
Since I keep seeing people share the same article over and over again, I want you to think critically for a moment.
This is a gesundheit, which they claim shows proof of masks working as source control of aerosol emissions.
Let me know if you spot the error.Hint 👇🏻👇🏻👇🏻
1/2 pic.twitter.com/aXmTAt4ElH— Megan Mansell (@mamasaurusMeg) January 25, 2023

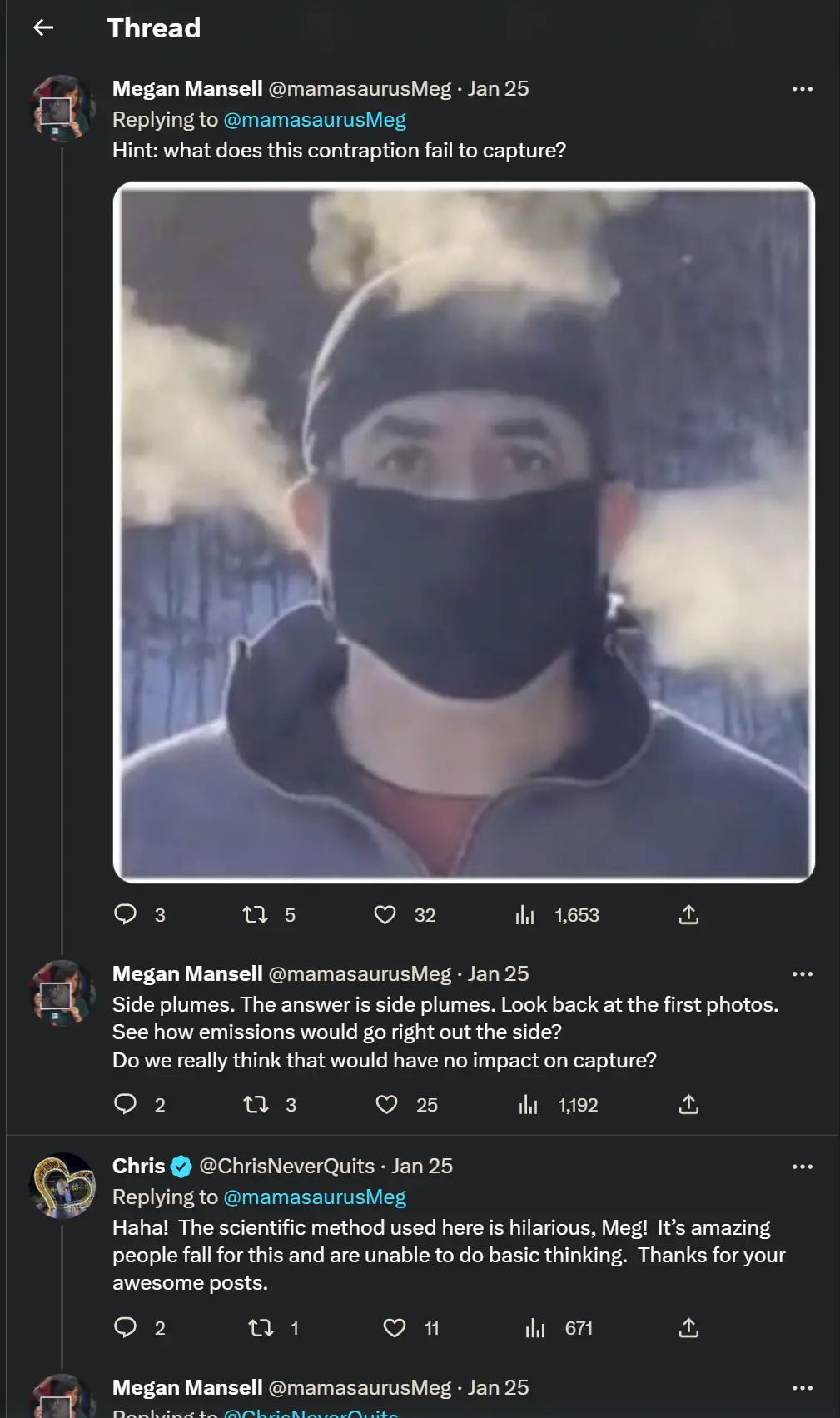
While the Department of Health and Human Services’ fact sheet on N95s says they “can” filter particles under 0.3 microns, which can include SARS-CoV-2, Mansell said they aren’t rated to capture matter below that threshold.
The sheet also warns N95s can’t filter gases and vapors, which include aerosolized COVID, and N95 maker Honeywell sets the minimum at 0.3 microns as well, she said.
“More than 90% percent of exhaled particulates have been shown to fall under 0.3 µm,” Mansell’s essay says, citing a January study in Elsevier journal Environmental Research. Such small matter can stay aloft for “hours, even days, depending on air exchange rates within the given space,” she wrote, citing a National Institute of Allergy and Infectious Diseases research letter to the New England Journal of Medicine.
The claim that N95s actually filter better under that threshold depends on a misunderstanding of Brownian motion, which “only occurs when there is essentially no velocity,” such as between breathing in and out, Mansell said.
